Seated Male Figurine - 2500-900
This section collects any data citations, data availability statements, or supplementary materials included in this article.

Thank you for your valuable comment. Regarding your suggestion about the data presented on lines 390-443, we understand your perspective about not presenting all results, particularly those deemed less critical to the main conclusions. Your concern about the potential burden on the readers is duly noted. However, our intention behind presenting these results in detail was driven by a strong commitment to transparency and consistency. Our aim was to provide a comprehensive overview of all the data and outcomes we obtained during our study. We believe that every reader, with varying interests and focus points, might find different parts of the results relevant. Thus, providing a complete set of results could serve to meet the diverse needs of our audience. We understand the importance of maintaining a balance between detail and brevity to not overburden the reader. In response to your comment, we will undertake a careful review of the specified section to ensure it is as concise and reader-friendly as possible while still maintaining the comprehensive presentation of our results.
Thank you for taking the time to review our manuscript and for your insightful comments. Your feedback is instrumental in refining the quality of our work, and we greatly appreciate your suggestions on how to clarify the presentation and interpretation of our statistical analyses.
Project registration, associated dataset and JASP outputs for all performed analyses are available at the Open Science Framework [OSF] repository (URL: https://osf.io/bjecr; DOI: https://doi.org/10.17605/OSF.IO/BJECR).
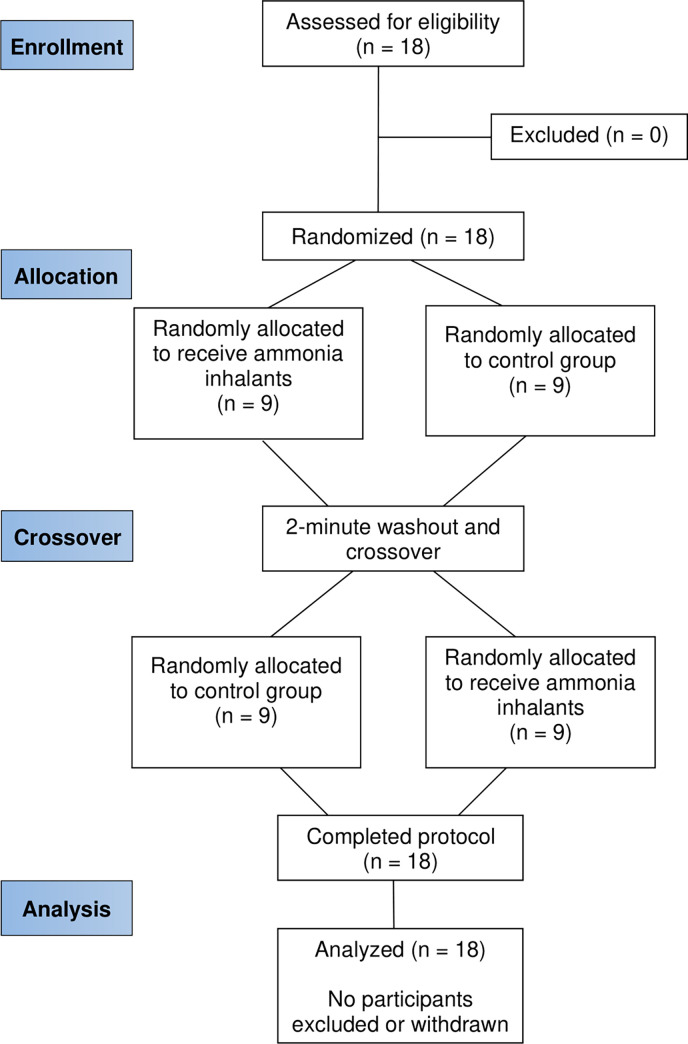
Furthermore, our study encountered some logistical constraints that determined the number of participants we could feasibly accommodate. Our sample size was limited to 18 participants due to the maximal capacity of the sleep laboratory we utilized for this research. The laboratory could only accommodate six subjects in one testing session, which created a practical ceiling on the number of individuals who could participate simultaneously.
I suggest that the conclusion needs to be reformulated; there is no need to repeat the results in this section and with the same abbreviations, (e.g. ammonia inhalant markedly improved the reaction time, jumping, and sensation of pain of soldiers). It should conclude the main results in a good manner. In addition, it should be tempered (e.g. in similar testing conditions of prolonged sleep deprivation). It should also finish with a recommendation for future studies about this topic (e.g., Further investigations including females and using different tests are needed…)
Thank you for highlighting the limitations that might influence the conclusions of our study. Your input regarding the sample size, absence of blinding, and the lack of qualitative and quantitative evaluation of sleep is very much appreciated.
-L164-168: This paragraph should clearly describe the objectives of the study: TSD (36 h), cognitive (SRT…) physical (JH) military personnel (18 male).
Thank you for your suggestion to replace "incorrect trials" with "incorrect detections" for greater clarity. However, we respectfully disagree with this recommendation in the context of our study. In the case of simple reaction time tasks, the term "trial" refers to each individual attempt or response made by the participant. Therefore, "incorrect trials" accurately reflects the number of times the participants made incorrect responses during the task.
-L139: I suppose that this study is very interesting about this topic and it could be added as a recent reference (Repeated low-dose caffeine ingestion during a night of total sleep deprivation improves endurance performance and cognitive function in young recreational runners: A randomized, double-blind, placebo-controlled study (2022))
Thank you for your insightful suggestion about monitoring participants' sleep quality and quantity. We actually collected such data using actigraphs and polysomnography throughout the study, and participants completed various sleepiness scales and sleep habit forms. However, we decided not to include these findings as we consider them beyond the scope of this particular paper. However, we are working on another, more comprehensive manuscript that includes these data on a larger scale.
Although there were detrimental effects of TSD, the usage of AI did not reduce those adverse effects. However, regardless of TSD, AI did result in a short-term increase in HR, improved SRT without affecting the number of errors, and improved JH while concurrently decreasing the RPE. No changes, yet, were observed in SA and DAS. These results suggest that AI could potentially be useful in some military scenarios, regardless of sleep deprivation.
The protocol for disassembling and reassembling a military-standard issue assault rifle (specifically the Czech vz. 58 assault rifle) was selected to assess changes in manual dexterity as it is representative tasks that soldiers may encounter in field operations [46]. During the protocol, participants were tasked to disassemble and reassemble a rifle consisting of 8 parts as fast as possible. Prior to the task’s onset, standing participants were instructed to place their hands behind their backs and wait for the researcher’s "start" command, after which they attempted to disassemble the rifle as quickly as possible. After a two-minute break, during which participants organized the rifle parts on a table, they then proceeded to reassemble the rifle under the same instruction, and the time was recorded. During the reassembling, the final step was conducting a successful "rifle function check". The time for completion of the task was measured using a handheld stopwatch and recorded on a digital camera for possible corrections.
In response to your comments, we have incorporated additional text in the manuscript. For the sample size, we agree that a larger and more diverse cohort would provide a more comprehensive view. However, we had 18 participants for logistical and resource reasons, which we believe is adequate as substantiated by the sensitivity analysis described in our statistics section. As for the lack of blinding, we acknowledge that blinding is a crucial element in many experimental designs. However, due to the nature of the study and the use of ammonia inhalants, blinding was not feasible. We have added a text in the limitations section to further elaborate on this point. While we do possess qualitative and quantitative sleep evaluation data, we chose not to include them in this manuscript. Our decision was guided by considerations for readability and consistency. Furthermore, we're currently preparing a more extensive manuscript where these data, including findings from actigraphy, will be thoroughly presented and discussed. Including them here might lead to instances of double-publishing, which we aim to avoid. This strategic limitation is included in our manuscript (see lines 746 to 770 in the revised manuscript). We sincerely appreciate your thoughtful suggestions and believe that the clarifications added in response to your points will provide a more accurate and comprehensive perspective for our readers.
- Line 79 (also Line 173): I suggest replacing “cadets” because it is with double meaning, or explaining it in parentheses (“young armed”, “police force”) to avoid confusion.
During the entire study protocol, participants received personalized daily food rations consisting of standard ’ready to eat’ meals commonly used in the Czech military. One week before the experiment, participants’ body composition was measured (using air displacement plethysmography; Bod Pod Body Composition System; Life Measurement Instruments, Concord, CA), and the total daily energy expenditure was derived from the estimated resting metabolic rate and application of an "active" physical activity factor of 1.6 [37] to the individual caloric requirements. In addition, each participant was allowed ad libitum water consumption. Breakfast was consumed at ~09:30 h, lunch at ~12:30 h, and dinner at ~17:30 h, each day (Fig 2). Additionally, all forms of stimulants were prohibited 72 hours before and during the testing protocol.
In sum, despite the consistency of our findings with those of the prior investigation, it is imperative to consider that the regulation of HR is predominantly controlled by the autonomic nervous system and the opposing actions of its sympathetic and parasympathetic components. This constitutes a complex system that may be impacted by various confounding factors during the prolonged experiments, as were conducted in this study, such as dietary intake, energy balance, hydration, physical activity, effect of shooting stress, temperature regulation, and psychological stress. Thus, the following potential studies should consider testing cardiovascular responses throughout the whole study period.
To sum up, when considering our data and the data from previous studies collectively, AI may positively impact explosive performance, regardless of the individual’s sleep status. Our results also indicate that this effect may have some transfers to real-world dynamic exercises, such as jumping performance. Consequently, even though a decrease in RPE after the physical performance and improvement in short-term movements, such as jumping over a barrier or sprinting across a battlefield, may even have life-or-death consequences in military contexts, it is still necessary to take these results with caution. There is currently a shortage of published research examining the effect of AI on performance, and further research in this area is necessary to establish a more robust evidence base regarding its effect.
We have incorporated your comment into our revisited manuscript and added the following text: "Furthermore, multiple reviews and meta-analyses (28) show the potential positive effects of caffeine are likely to manifest about 1 hour after ingestion relative to, which may not be sufficient if immediate assistance is required.”
Do you want your identity to be public for this peer review? For information about this choice, including consent withdrawal, please see our Privacy Policy.
4. We note that the original protocol that you have uploaded as a Supporting Information file contains an institutional logo. As this logo is likely copyrighted, we ask that you please remove it from this file and upload an updated version upon resubmission.
Although previous studies have investigated the effects of total sleep deprivation and AI independently, none included the combination of these conditions. Furthermore, these studies all used various measuring techniques (CMJ with arm movement vs without; peak jump height vs average jump height; different rest periods between jumps; estimated power output vs direct assessment, etc.), all of which can impact the data, decreasing comparativeness of their findings to ours. Therefore, we acknowledge that the data from those studies bring interesting insights, but more studies with consistent methodology are still needed in order to make justifiable comparisons.
Thank you for your suggestion. We agree that explicitly stating the objectives could provide clarity. However, we believe that providing this information too early might potentially disrupt the flow of the introduction. As this information is comprehensively detailed in the methods section just a few paragraphs later, we have decided to maintain the current structure to ensure a smooth reading experience. We appreciate your valuable insight and will consider this feedback for future manuscripts.
Our results also suggest that using AI may enhance performance in CMJ height by 1.5% and concurrently reduces RPE by 9.4%, regardless of total sleep deprivation. Notably, the observed improvements may be attributed to the psychological arousal effects of AI, such as heightened alertness, which have been documented in previous research [32, 35]. This phenomenon commonly referred to as the "psyching-up" effect of AI, may enhance short-term performance by activating the sympathetic branch of the autonomic nervous system and increasing psychological activation [29]. Based on that, previous studies showed an increased peak rate of force development during the isometric mid-thigh pull exercise [31, 33], an explosive isometric strength task using a slow stretch-shortening cycle, the same as during CMJ. Additionally, the usage of AI increased power output over repeated high-intensity sprint exercises [35]. Regarding the following facts, while assuming a correlation between CMJ performance and short sprints [84], the usage of AI may have potential applications in some specific military scenarios, but more studies delineating optimum protocols and delivery methods are necessary.
On the other hand, the term "detections" typically implies the identification or recognition of specific stimuli or targets. This terminology is more commonly used in tasks such as signal detection or target identification. In our study, the focus was on the accuracy of the participants' overall responses, rather than specifically detecting or recognizing stimuli.
-L143: “The potential positive effects of caffeine are likely to manifest about 1 hour after ingestion relative to many reviews and meta-analysis (and not between 10 and 60 min) (Reference: Grgic J, Grgic I, Pickering C, et al. Br J Sports Med 2020;54:681–688)
Each participant completed two trials of rifle disassembly and reassembly (AI and CON, in a randomized order) with two minutes of rest between conditions. The performance measure used in this study was the sum of the disassembly and reassembly time in seconds for each condition (AI and CON).
Furthermore, to emphasize the participants' prior experience with sleep deprivation, we have added the following statement in the Participants section: "Additionally, the participants selected for this study were well-acquainted with total sleep deprivation, having experienced it during their military duties previously." We believe these statements adequately address the familiarization with both the experimental process and sleep deprivation.
Thank you for your valuable suggestion on tempering our conclusion. In line with your feedback, we have revised the text accordingly. It now reads: "These results suggest that AI could potentially be useful in some military scenarios, regardless of sleep deprivation." This new phrasing more accurately reflects our findings.
-L252: It is useless to rewrite “in a randomized order” because it was already stated in the methods section. (To be corrected throughout this section)
For ESS, we observed statistically significant main effect of time (F4 450.572 = 39.764, pbonf < 0.001, η2 = 0.701), indicating a statistically significantly greater sleepiness score at -24 compare to 0 (mean difference = 11.72, pbonf < 0.001, Cohen’s d = 2.91 [1.25, 4.58]), -12 (mean difference = 9.11, pbonf < 0.001, Cohen’s d = 2.26 [0.87, 3.65]), -36 (mean difference = 3.94, pbonf = 0.018, Cohen’s d = 0.98 [0.03, 1.93]), and +8 (mean difference = 10.89, pbonf < 0.001, Cohen’s d = 2.70 [1.13, 4.28]) (Fig 7A).
There was also a statistically significant condition × time span interaction (F4, 212.765 = 22.593, pbonf < 0.001, η2 = 0.009) (Fig 4B), demonstrating that after using AI we observed the highest heart rate at AI 0–15 compare to baseline (mean difference = 22.95 bpm, pbonf < 0.001, Cohen’s d = 2.08 [0.68, 3.47]), AI 15–30 (mean difference = 6.13 bpm, pbonf < 0.001, Cohen’s d = 0.55 [0.09, 1.02]), AI 30–45 (mean difference = 10.28. bpm, pbonf < 0.001, Cohen’s d = 0.93 [0.26, 1.60]), and AI 45–60 (mean difference = 13.00 bpm, pbonf < 0.001, Cohen’s d = 1.18 [0.35, 1.99]). Without the use of AI we observed highest heart rate in CON 0–15 compare to baseline (mean difference = 17.07 bpm, pbonf < 0.001, Cohen’s d = 1.54 [0.49, 2.60]), CON 15–30 (mean difference = 4.29 bpm, pbonf < 0.001, Cohen’s d = 0.39 [0.01, 0.77]), CON 30–45 (mean difference = 7.16 bpm, pbonf < 0.001, Cohen’s d = 0.65 [0.14, 1.16]), and CON 45–60 (mean difference = 9.43 bpm, pbonf < 0.001, Cohen’s d = 0.85 [0.30, 1.45]).
This study was supported by the Charles University Grant Agency (GAUK 986120), the SVV research program (SVV 2020-2022-260599), the Cooperatio Program (SPOB research area) and the Ministry of Health of the Czech Republic (MH CZ-DRO; NUDZ, 00023752). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
[NOTE: If reviewer comments were submitted as an attachment file, they will be attached to this email and accessible via the submission site. Please log into your account, locate the manuscript record, and check for the action link "View Attachments". If this link does not appear, there are no attachment files.]
1. Please ensure that your manuscript meets PLOS ONE's style requirements, including those for file naming. The PLOS ONE style templates can be found at
4. We note that the original protocol that you have uploaded as a Supporting Information file contains an institutional logo. As this logo is likely copyrighted, we ask that you please remove it from this file and upload an updated version upon resubmission.
Eighteen healthy male military cadets (age = 24.1 ± 3.0 years, height = 181.5 ± 6.3 cm, weight = 79.3 ± 8.3 kg, 4.0 ± 0.9 total years of service, all measurements reported as mean ± SD) serving at the Military department of Charles University participated in this study. The cadets were selected (Q1, 2021) primarily due to their homogenous and synchronized daily cycle based on mandatory morning lineups and the University program. Eligible participants were required to have passed an annual physical fitness test and medical checkup within the last year, have at least two years of active-duty service experience, report a high level of comfort handling firearms, be non-smokers, and currently not working shiftwork or taking medications known to interfere with sleep, cognitive or physical performance. Additionally, the participants selected for this study were all well-acquainted with total sleep deprivation, having experienced it during their military duties. Prior to the study onset, all participants were fully informed about the experimental design and potential risks associated with participation, and provided written informed consent in accordance with the Declaration of Helsinki.
Thank you for your keen observation, we have added "as control" before introducing the abbreviation (CON) in the revised manuscript.
L116, 117: The sentence should be reformulated; I suggest this correction; to various “physical”, cognitive, and behavioral impairments, such as fatigue and “decreased” attention and reaction time.
Data from this study are part of a broader research project aimed at investigating the effects of different light conditions on cognitive and physiological performance during periods of total sleep deprivation. We used a crossover randomized controlled trial design with within-subject repeated-measures to assess the effects of ~36 hours of total sleep deprivation and acute ammonia inhalation on occupationally relevant military tasks in military personnel.
Additionally, we sourced our participants from a cohort of cadets at the Military department, which also has its own capacity constraints. To maintain the standardization of the study, we aimed to test participants with similar daily routines. We specifically sought to include participants within a short period around the equinox to account for any seasonal variations that could impact the circadian rhythms. This intention was to minimize the potential influence of individual lifestyle differences and external factors related to seasonal changes on the study results.
We sincerely thank you for your constructive feedback on our conclusion section. Your suggestion to refrain from repeating the results verbatim, temper the interpretation, and include recommendations for future research was truly insightful.
Authors found that there was no condition and time interaction in any test, but there was faster Reaction Time without increasing the number of errors, higher Jump height, lower RPE, and higher Heart Rate after using Ammonia Inhalants compared to Control regardless of Total Sleep Deprivation.
Thank you for your suggestion to use "psycho-stimulant" instead of "stimulant". However, to avoid potential confusion or debate over the distinction between these two terms, we have chosen to eliminate the word "stimulant" entirely from the revised manuscript.
When you resubmit, please ensure that you provide the correct grant numbers for the awards you received for your study in the ‘Funding Information’ section.
In accordance with your recommendations, we have restructured our conclusion. We've incorporated a tempered discussion of our main findings while emphasizing the study's specific context, and concluded with recommendations for future investigations.
If your institution or institutions have a press office, please notify them about your upcoming paper to help maximize its impact. If they’ll be preparing press materials, please inform our press team as soon as possible -- no later than 48 hours after receiving the formal acceptance. Your manuscript will remain under strict press embargo until 2 pm Eastern Time on the date of publication. For more information, please contact onepress@plos.org.
2 We note that the grant information you provided in the ‘Funding Information’ and ‘Financial Disclosure’ sections do not match.
Many occupations that require prolonged periods of wakefulness, including soldiers, also demand the ability to maintain manual dexterity. Previous research has indicated that impaired manual dexterity can be observed after 24 h of total sleep deprivation among medical professions [76]. As previously discussed, while AI has been assumed to be an effective countermeasure for preserving vigilance and attention [29], concerns have arisen about its potential adverse effects on tasks involving manual dexterity, particularly in terms of increased tearfulness or hand tremors—a typical reaction to inhalations of AI. However, in our results we did not observe any impact on rifle disassembly and reassembly time as a result of total sleep deprivation or the usage of AI. The current findings align with the results of previous studies that have been conducted on military personnel, demonstrating that a 24 h period of total sleep deprivation did not impact the manual dexterity in rifle disassembly and reassembly [77] or the laboratory-based Grooved Pegboard test [78].
The disparities between studies outcomes may likely be attributed to the various methods used for measuring manual dexterity in medical personnel, such as the virtual laparoscopy simulator, or to the possibility of movement automation that soldiers may develop as a result of frequent repetition of tasks during their service, referred to as a "drill." Although the present study did not specifically evaluate variables as hand steadiness, but only total time to finish a task, collectively, the evidence suggests that neither total sleep deprivation nor usage of AI has an impact on manual dexterity in military personnel.
Thank you for your suggestion to replace "condition" with "ammonia" for greater clarity. While we appreciate your input, we respectfully disagree with this recommendation.
- L99: I suppose that “short-term increase in HR” should not be stated in the conclusion because it is not a performance improvement (we focus only on important results about the subject: impact of AI on performance during TSD at least in the conclusion)
- L104: I suppose that there is a lack of general introduction concerning the disrupted sleep-wake cycle in everyday life (stress, shift work, jetlag…) before moving on to the part that specifies its relation with the military.
- I suggest that this section should be rewritten in a more precise way. It should focus on essential results about the main subject: the impact of TSD on the tests selected, and the impact of AI on performance tests (by describing the scientific reasons about previous similar works, without repeating results or useless information).
A lack of sleep can pose a risk during military operations due to the associated decreases in physical and cognitive performance. However, fast-acting ergogenic aids, such as ammonia inhalants (AI), may temporarily mitigate those adverse effects of total sleep deprivation (TSD). Therefore, the present study aimed to investigate the acute effect of AI on cognitive and physical performance throughout 36 hours of TSD in military personnel.
If your institution or institutions have a press office, please let them know about your upcoming paper now to help maximize its impact. If they'll be preparing press materials, please inform our press team within the next 48 hours. Your manuscript will remain under strict press embargo until 2 pm Eastern Time on the date of publication. For more information please contact onepress@plos.org.
We used unloaded countermovement jump (CMJ), one of the most common and straightforward strategies to monitor short-term neuromuscular performance in tactical populations [43]. Each CMJ session included 2 sets (AI and CON in a randomized order) of 3 maximal effort CMJs with 2 min of inter-set standing rest. The researcher verbally instructed and encouraged the participants to jump as high as possible on each jump. All CMJs were performed with wooden dowel (~ 0.5 kg) as a mock barbell placed across the participant’s upper back mimicking a regular back squat. A linear position transducer (GymAware Power Tool; Kinetic Performance Technologies, Canberra, Australia) was attached to both sides of a dowel to measure the performance. The depth of the CMJ depth was self-selected. Participants wore the same sports t-shirts, shorts and shoes during each test period. The mean of the 3 jump heights (cm) was calculated for each condition at each test session.
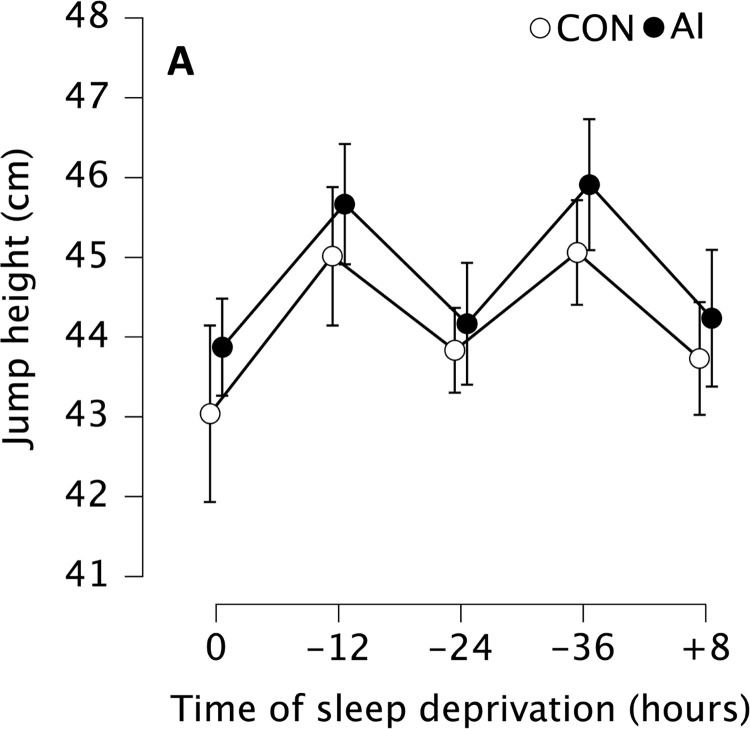
Data are presented as mean (circles) and error bars represent their 95% confidence interval (LL, UL) at baseline after a full night of sleep (0 h), after 12 (-12 h), 24 (-24 h) and 36 (-36 h) hours of total sleep deprivation followed by 8 (+8 h) hours of recovery sleep.
Thank you for your observation regarding the repetition. However, we have chosen to retain this phrase in certain sections to continually remind readers about the randomization of the procedure, which is a key aspect of our study design. This choice was made to reinforce the study's methodological rigor and prevent potential confusion. We hope this explanation helps, and we value your thoughtful feedback.
Thank you for pointing out the need to define “pbonf” at its first appearance. We have revised the text to clarify this term. The first sentence (at line 346) now reads: “When the ANOVA tests demonstrated a statistically significant condition × time (× time spans or × percentage difference) interaction or a statistically significant main effect for condition, time, time spans, or percentage difference, post-hoc comparisons of the mean differences were performed using the Bonferroni correction (pbonf).”
- L116, 117: The sentence should be reformulated; I suggest this correction; to various “physical”, cognitive, and behavioral impairments, such as fatigue and “decreased” attention and reaction time.
Please review your reference list to ensure that it is complete and correct. If you have cited papers that have been retracted, please include the rationale for doing so in the manuscript text, or remove these references and replace them with relevant current references. Any changes to the reference list should be mentioned in the rebuttal letter that accompanies your revised manuscript. If you need to cite a retracted article, indicate the article’s retracted status in the References list and also include a citation and full reference for the retraction notice.
A simple reaction time test was used to assess the speed of responses to visual stimuli [39]. The evaluation of reaction time was performed using the Psychology Experiment Building Language (PEBL Version 2.0) software [40]. The test consists of instantaneous responses to a visual stimulus by pressing a spacebar key on a laptop’s keyboard as quickly as possible when a visual stimulus (white letter X in the middle of the black screen) appears. In the test, 50 trials of stimuli were presented with an interstimulus interval that randomly varied between 250 ms and 2500 ms. Each participant completed four tests (each time two, either with AI or CON, in randomized order) with 2 minutes of inter-test rest. The simple reaction time data obtained were inspected according to pre-determined criteria, which excluded trial executions that were deemed incorrect due to a reaction time shorter than 150 ms or longer than 3000 ms. The mean reaction time (measured in milliseconds) and the number of incorrect trial executions were used as the variables in the subsequent statistical analysis.
The PLOS Data policy requires authors to make all data underlying the findings described in their manuscript fully available without restriction, with rare exception (please refer to the Data Availability Statement in the manuscript PDF file). The data should be provided as part of the manuscript or its supporting information, or deposited to a public repository. For example, in addition to summary statistics, the data points behind means, medians and variance measures should be available. If there are restrictions on publicly sharing data—e.g. participant privacy or use of data from a third party—those must be specified.
Thank you for your suggestion to start with the quality measured by each test (accuracy, speed, strength) and the type of test (cognitive, physical, psychological) prior to describing the tests in detail. We appreciate your attention to the clarity of our methodology. However, we have chosen to describe the tests chronologically, consistent with the figure that outlines the order of the tests. We believe that this approach will help readers understand the sequence of events in our study and prevent any potential confusion. We hope this clarifies our decision, and we appreciate your thoughtful feedback.
In the case of jump height, we observed statistically significant main effect of time (F4, 29.447 = 8.070, pbonf < 0.001, η2 = 0.035). In subsequent post-hoc tests, the jump height was statistically significantly higher in the evenings compare to the mornings. Particularly -12 was higher than 0 (mean difference = 1.88 cm, pbonf = 0.015, Cohen’s d = 0.33 [0.22, 0.65]), -24 (mean difference = 1.33 cm, pbonf = 0.010, Cohen’s d = 0.24 [-0.05, 0.52]), +8 (mean difference = 1.35 cm, pbonf = 0.046, Cohen’s d = 0.24 [-0.05, 0.53]), and also -36 was higher compare to 0 (mean difference = 2.03 cm, pbonf = 0.006, Cohen’s d = 0.36 [-0.04, 0.67]) and -24 (mean difference = 1.50 cm, pbonf = 0.014, Cohen’s d = 0.26 [-0.28, 0.56]) (Fig 6).
PLOS ONE does not copyedit accepted manuscripts, so the language in submitted articles must be clear, correct, and unambiguous. Any typographical or grammatical errors should be corrected at revision, so please note any specific errors here.
Participants were administered a standardized sleepiness scale and underwent simple reaction time testing, handgun shooting accuracy protocol, a rifle disassembly and reassembly protocol, and countermovement jump testing at each testing session. Participants performed each individual test twice at each testing period, either with AI (AI) or without AI (CON), in randomized order (Fig 1) and separated by 2 minutes of rest (in order to minimize any potential carryover effects of the AI) [31].
Despite this, our results suggest that the utilization of AI may be beneficial for soldiers, as it may improve their SRT without increasing the number of errors, regardless of the level of total sleep deprivation. In military contexts, where performance demands are high and have significant implications for many individuals’ well-being, SRT can be a critical determinant of success or failure and may even have life-or-death consequences [61]. To sum up, even though it must be taken into account that the difference we observed was on the order of milliseconds, the utilization of AI may have potential applications in specific military scenarios, no matter the length of sleep deprivation.
Thank you for suggesting the inclusion of this recent study. We agree that it's a valuable reference for our topic. We have now added the text "and exhaustive time on 400-meter run by 10%" to our manuscript, citing the recommended study.
7. PLOS authors have the option to publish the peer review history of their article (what does this mean?). If published, this will include your full peer review and any attached files.
Thank you for your suggestion regarding the reporting of unchanged results in the conclusion. While we appreciate your input, we believe it's essential to maintain transparency by presenting all our findings, regardless of whether they show change or not. Our intention is to provide a complete view of our experiment, which includes the unchanged variables. We, therefore, decided not to remove this information from the conclusion.
For all AI trials, a capsule containing 0.3 mL of AI (composed of 15% of ammonia and 35% of alcohol) [36] was used according to the manufacturer’s instructions (Dynarex Corporation, Orangeburg, NY). When the ammonia fumes were released, researcher immediately held the capsule under the participant’s nose to inhale until a voluntary withdrawal reflex was observed [31].
A rebuttal letter that responds to each point raised by the academic editor and reviewer(s). You should upload this letter as a separate file labeled 'Response to Reviewers'.
A rebuttal letter that responds to each point raised by the academic editor and reviewer(s). You should upload this letter as a separate file labeled 'Response to Reviewers'.
PONE-D-23-07437R1Effects of 36 hours of sleep deprivation on military-related tasks: can ammonium inhalants maintain performance?PLOS ONE
We observed statistically significant main effect of time (F2.844, 10.030 = 10.478, pbonf < 0.001, η2 = 0.282, with Greenhouse-Geisser correction) indicating that soldiers reported highest RPE at -24 compare to 0 (mean difference = 1.11, pbonf < 0.001, Cohen’s d = 1.19 [0.32, 2.06]), -12 (mean difference = 1.03, pbonf = 0.010, Cohen’s d = 1.10 [-0.26, 1.93]), and +8 (mean difference = 0.86, pbonf = 0.002, Cohen’s d = 0.92 [0.14, 1.70]).
Yes, we indeed calculated the mean energy intake per day for each participant. However, as part of a larger research project, we are in the process of preparing another manuscript that focuses on the effects of sleep deprivation on hunger levels, among other variables. To avoid redundancy and possible data saturation, we decided not to include this specific piece of information in the current study. We believe that including the data on energy intake here could potentially overshadow the main findings of our study. However, we assure you that we have carefully monitored and accounted for this variable during our experiment. We hope this clarification meets your understanding.
The authors confirm that all ongoing and related trials for this drug/intervention are registered, including registration on ClinicalTrials.gov under the identifier number NCT05868798. The project was not preregistered as it was not a common practice in the field at the time of the project’s development and data collection.
A marked-up copy of your manuscript that highlights changes made to the original version. You should upload this as a separate file labeled 'Revised Manuscript with Track Changes'.
-L705: Some limitations of the study were not stated although they could influence the conclusions; the sample size is quite small; 18 and only men were used), the experimental protocol was not blinded, and qualitative and quantitative evaluation of sleep were not carried out.
- L103: keywords are not well selected; I suggest adding Performance (not tests), Ammonia Inhalants (not Ergogenic Aids), Soldiers or Army (not both), and Sleep Deprivation (not sleep loss).
In the present study, it is challenging to differentiate the various effects of HR as an indicator of physiological exertion or mechanical perturbation. This intra-individual variability may be attributed to the heightened mechanical impact of the heartbeat on shooting dynamics or may indicate an "over-arousal" that results in a decrease in performance, as demonstrated by the Yerkes-Dodson performance-arousal curve [75]. With all these points in mind, further research should delve into the interaction between these mechanical, physiological, and psychological factors that influence shooting more deeply to better understand the interplay of these elements. In summary, this study highlights that although AI did not improve handgun shooting accuracy, it was posed no negative effect either. It is still important to keep in mind the parameters of our study (observed effect sizes). However, the unaffected shooting accuracy, combined with the decreased SRT noted in the previous section, can be relevant in real-life military contexts where a soldier may need to react quickly and shoot accurately.
-L319-323: The familiarization information should be written in the methods section. In this section, we only describe the realization of the test.
Thank you for submitting your manuscript to PLOS ONE. After careful consideration, we feel that it has merit but does not fully meet PLOS ONE’s publication criteria as it currently stands. Therefore, we invite you to submit a revised version of the manuscript that addresses the points raised during the review process.
Where the interaction effect was significant, we have provided an in-depth interpretation of these results, as you suggested. We refrained from testing or reporting the main effects in these cases, as per your advice.
The manuscript must describe a technically sound piece of scientific research with data that supports the conclusions. Experiments must have been conducted rigorously, with appropriate controls, replication, and sample sizes. The conclusions must be drawn appropriately based on the data presented.
This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Eighteen male military cadets (24.1 ± 3.0 y; 79.3 ± 8.3 kg) performed 5 identical testing sessions during 36 hours of TSD (after 0 [0], 12 [–12], 24 [–24], and 36 [–36] hours of TSD), and after 8 [+8] hours of recovery sleep. During each testing session, the following assessments were conducted: Epworth sleepiness scale (ESS), simple reaction time (SRT), shooting accuracy (SA), rifle disassembling and reassembling (DAS), and countermovement jump height (JH). Heart rate (HR) was continuously monitored during the SA task, and a rating of perceived exertion (RPE) was obtained during the JH task. At each time point, tests were performed twice, either with AI or without AI as control (CON), in a counterbalanced order.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
There was also statistically significant main effect of condition (F1, 1060.42 = 9.40, p = 0.007, η2 = 0.014), demonstrating that application of AI reduced simple reaction time (mean difference = 4.85 ms, pbonf = 0.007, Cohen’s d = 0.19 [0.04, 0.34]) (Fig 3A).
An invoice for payment will follow shortly after the formal acceptance. To ensure an efficient process, please log into Editorial Manager at http://www.editorialmanager.com/pone/, click the 'Update My Information' link at the top of the page, and double check that your user information is up-to-date. If you have any billing related questions, please contact our Author Billing department directly at authorbilling@plos.org.
Considering these factors, we believe that using "incorrect trials" is appropriate and clearer in the context of our study. We appreciate your suggestion and value your input in improving the clarity of our manuscript.
Authors found that there was no condition and time interaction in any test, but there was faster Reaction Time without increasing the number of errors, higher Jump height, lower RPE, and higher Heart Rate after using Ammonia Inhalants compared to Control regardless of Total Sleep Deprivation.
The associated dataset and JASP outputs for all performed analyses are available at the Open Science Framework [OSF] repository (URL: https://osf.io/3rj84/; DOI 10.17605/OSF.IO/3RJ84).
This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Despite these fairly straightforward findings, some observations in our study diverged from previous findings. For example, one study shows that shooting accuracy decreased as HR increased in standing positions [73], but another study suggests that low-intensity exercise, which leads to commensurate increases in HR, may initially enhance shooting accuracy before a decline is observed. Nonetheless, the different outcomes observed could be attributed to the substantial intra-individual variability in managing psychological factors, such as fatigue and stress, which may impact HR and, consequently, shooting accuracy among individuals [74]. Therefore, while our results agree with previous research [16, 72] that also evaluated shooting accuracy using small arms simulators rather than live fire, it is crucial to acknowledge that the use of simulated weapons in evaluating shooting performance may affect the applicability of the findings to real-life military situations [74].
To assess the reliability of the task, participants familiarize themselves with the disassembly and reassembly protocol before the study begins. They repeatedly performed the protocol for three consecutive days, one week before participating in the study. Their performance showed sufficient reliability (data and reliability analysis of the familiarization period can be found in the supplementary materials).
The manuscript must describe a technically sound piece of scientific research with data that supports the conclusions. Experiments must have been conducted rigorously, with appropriate controls, replication, and sample sizes. The conclusions must be drawn appropriately based on the data presented.
Despite the relatively small sample size, we believe the homogeneity of the participants and the tightly controlled conditions under which the study was conducted add some robustness to the reliability of our findings. Nevertheless, we recognize the benefit of a larger and more diverse sample size in future studies to enhance the generalizability of our findings.
Do you want your identity to be public for this peer review? For information about this choice, including consent withdrawal, please see our Privacy Policy.
Please use the space provided to explain your answers to the questions above. You may also include additional comments for the author, including concerns about dual publication, research ethics, or publication ethics. (Please upload your review as an attachment if it exceeds 20,000 characters)
Reviewer #2: A single cohort study of 18 healthy male cadets investigated the acute effects of ammonia inhalants (AI) versus control on cognitive and physical performance during a 36 hour period of total sleep deprivation (TSD). ANOVA methods were used to analyze the main objectives of the trial. The conclusions are unclear.
Thank you for your suggestion on revising the sentence structure. We value your input as we strive to make our manuscript as clear and reader-friendly as possible. However, for the sake of consistency throughout the text, we have decided to retain the current format. We believe this approach maintains the flow of the document and minimizes potential confusion. We hope you understand and thank you again for your valuable feedback.
Addressing your first point regarding the unclear conclusions, we have made substantial revisions to the discussion section to clearly elucidate our conclusions based on the data and statistical analyses. We believe that the revised manuscript now provides a coherent understanding of the study’s outcomes.
This study’s strengths comprise the tightly controlled protocol and crossover randomized controlled trial design, which allowed for direct within-subject repeated-measures investigation of the effects of total sleep deprivation and ammonia inhalation. However, study is not without limitations. For example, we were not able to perform any military-specific physically demanding tasks (e.g., casualty drag, wall climb, sprinting with personal protective equipment, loaded carries, etc.) because of limited space in the laboratory-based setup. Nevertheless, the CMJ is a commonly used physical task to assess explosive neuromuscular performance, and the linear position transducer that we used is a reliable and space friendly tool for assessing CMJ. Therefore, as AI increased CMJ height, increased HR, and improved SRT in our study, future researchers should investigate the effects of AI on more demanding military-specific tasks (or tasks that last longer than the CMJ) where increasing HR or improving SRT may help aid performance. Additionally, one limitation of this study was the absence of a placebo condition due to the distinct characteristics of AIs. Participants can likely distinguish AIs from any potential placebo due to their strong smell and immediate physical response after inhalation. Though some placebo substances like menthol oil or Vicks VapoRub have been used in other studies [29], these also have identifiable (though arguably less intrusive) smells that can potentially compromise the blinding process. Consequently, participants in our study likely knew when they were and were not inhaling an AI. Nonetheless, no studies have reported an increase in performance superior to AI inhalation for placebo or control conditions, indicating a limited placebo effect in this context.
Additionally, all heart rates in same time spans after AI administration were higher compared to CON. AI 0–15 was higher than CON 0–15 (mean difference = 5.88 bpm, pbonf < 0.001, Cohen’s d = 0.53 [0.13, 0.93]), AI 15–30 was higher than CON 15–30 (mean difference = 4.04 bpm, pbonf < 0.001, Cohen’s d = 0.36 [0.53, 0.68]), AI 30–45 was higher than CON 30–45 (mean difference = 2.76 bpm, pbonf < 0.001, Cohen’s d = 0.25 [0.01, 0.51]), AI 45–60 was higher than CON 45–60 (mean difference = 2.31 bpm, pbonf < 0.001, Cohen’s d = 0.21 [0.03, 0.45]) (Fig 4B).
The actual testing protocol began with a night of uninterrupted sleep from ~22:00 h to ~06:30 h. Participants then underwent 5 identical testing sessions from every ~07:30–09:30 h in the morning and ~19:00–21:00 h in the evening. The first test occurred in the morning after the full night of baseline sleep (0 h) and again after 12 hours (-12 h), 24 hours (-24 h), and 36 hours of total sleep deprivation (-36 h) followed by additional testing session after 8 hours (from 22:30 to 06:30 h) of recovery sleep (+8 h). During total sleep deprivation, participants were not allowed to sleep and were kept awake in a common room by passive means, such as playing board games, watching television and reading books while under constant supervision of the research team. Furthermore, the participants were subjected to a constant ambient room light for the entire duration of total sleep deprivation period.
Thank you for your comment to provide a more general introduction on the disrupted sleep-wake cycle. To address this, we have included a new section of following text in our introduction:
Thank you for outlining the additional requirements necessary for the revision of our manuscript. We appreciate your guidance on adhering to PLOS ONE's specific standards.
-L705: Some limitations of the study were not stated although they could influence the conclusions; the sample size is quite small; 18 and only men were used), the experimental protocol was not blinded, and qualitative and quantitative evaluation of sleep were not carried out.
-L252: It is useless to rewrite “in a randomized order” because it was already stated in the methods section. (To be corrected throughout this section)
Thank you for your valuable feedback on our manuscript. We appreciate your detailed comments regarding the methodology, study limitations, and conclusions. We acknowledge the importance of these issues and commit to making the necessary modifications in our revised manuscript. We believe the inclusion of your suggestions enhanced the rigor of our work.
(A) Schedule for days 0–3 of the study, with testing session times (indicated by arrows) at baseline after a full night of sleep (0 h), after 12 (-12 h), 24 (-24 h) and 36 (-36 h) hours of total sleep deprivation followed by 8 (+8 h) hours of recovery sleep. (B) Daily timeline of the study. DAS protocol = rifle disassembly and reassembly protocol; #During the total sleep deprivation period between days 1 and 2, participants were not allowed to sleep. Sleep hours on nights leading into day 1 and 3 were from 22:00 h to 06:30 h.
-L196: Is there a familiarization (before the testing day) with the sleep deprivation (36 hours) to be familiar with the experimental process and the sleep adaptation? If yes, describe this familiarization.
- L99: I suppose that “short-term increase in HR” should not be stated in the conclusion because it is not a performance improvement (we focus only on important results about the subject: impact of AI on performance during TSD at least in the conclusion)
We’re pleased to inform you that your manuscript has been judged scientifically suitable for publication and will be formally accepted for publication once it meets all outstanding technical requirements.
We used Epworth Sleepiness Scale (ESS) translated into Czech. It is a self-administered eight-item questionnaire and takes two to three minutes to complete [38]. The questionnaire presents daily lifestyle activities (i.e. reading, watching TV etc.) and participants rate their current self-perceived likelihood of dozing off in each situation, from: “would never doze” (0) to “high chance of dozing” (3). The ESS provides a cumulative score between 0 and 24, with higher numbers indicating greater sleepiness.
Thank you for bringing this to our attention. We have amended the manuscript accordingly and replaced all instances of military time format with the standard scientific notation (i.e., 18:00 h).
Thank you for your suggestion. While VO2max is indeed an important measure, in this kind of studies, our primary focus was on cognitive and short-term physical variables. Given this focus, we did not consider VO2max a necessary measure for our research purposes. We appreciate your input and will certainly consider such aspects for future studies where long-term endurance might be more pertinent.
“Sleep is a fundamental yet often undervalued physiological process, indispensable for maintaining physical and mental well-being (1). It is an essential component of our circadian rhythms, which have been found to profoundly influence both cognitive and physical performance (2). However, these rhythms can easily be disrupted due to various factors such as stress, jetlag, travelling, or night-shift work. Such disruptions can result in cognitive and physical deficits, poorer mental health, and elevated health risks (3,4). Therefore, a deeper insight into the relationships between disruption to sleep and their combined effect on cognitive and physical performance is of paramount importance. This knowledge, while vital for all, may be especially critical for at-risk occupations such as military personnel. It has the potential to significantly influence their health and combat readiness (5). Given this, the optimization of health, well-being, and overall performance could be particularly crucial for them (6,7). The necessity of maintaining adequate sleep quality and quantity thus becomes evident, underscoring the integral role sleep plays in the well-being and performance of military personnel.”
The PLOS Data policy requires authors to make all data underlying the findings described in their manuscript fully available without restriction, with rare exception (please refer to the Data Availability Statement in the manuscript PDF file). The data should be provided as part of the manuscript or its supporting information, or deposited to a public repository. For example, in addition to summary statistics, the data points behind means, medians and variance measures should be available. If there are restrictions on publicly sharing data—e.g. participant privacy or use of data from a third party—those must be specified.
4. Protocol File: We have removed the institutional logo from the original protocol in the Supporting Information file due to copyright considerations and uploaded an updated version.
-L258: I suggest starting by giving the quality measured by the test (accuracy, speed, strength) and the type of test (cognitive, physical, psychological), before the description, and this for all 5 tests (for more clarity).
For the sum of the rifle disassembly and reassembly time there was no statistically significant main effect of time (F1, 1.362 = 0.098, pbonf = 0.759, η2 = 0.0008) nor the main effect of condition (F4, 10.825 = 0.754, pbonf = 0.560, η2 = 0.027). Descriptions of all results can be seen in the following table (Table 1).
For shooting accuracy, we observed no statistically significant main effect of time (F2.834, 35.844 = 1.755, pbonf = 0.171, η2 = 0.045, with Greenhouse-Geisser correction) or main effect of condition (F1, 27.222 = 1.529, pbonf = 0.233, η2 = 0.012).
Within one week, you’ll receive an e-mail detailing the required amendments. When these have been addressed, you’ll receive a formal acceptance letter and your manuscript will be scheduled for publication.
A laser-based simulator system (LASRX, Plano, TX & Beatrice, NE) with an infrared laser handgun (SIRT 110, Next Level Training, Ferndale, WA) was used (iron sights were used for aiming) to assess handgun shooting accuracy ([41], submitted). Each testing period included two trials of the laser-based handgun shooting protocol (either AI or CON, in randomized order). All trials were performed in the standardized isosceles high-ready stance position (i.e., feet parallel at shoulder-width with both arms extended, holding the handgun with outstretched arms and in front at eye level) [42]. For this study, a real-weight mock-up of the Czech military standard issue Glock 17/22 handgun was used (all participants were familiar with the handgun from their active service). Participants wore over-ear headphones during all testing procedures to hear the software command to start shooting and the simulated shooting blasts when pulling the trigger. A 20 cm circular target was placed on a blank wall 4 meters in front of the participants to simulate a standard-issue 50 cm target 10 meters away for the laser-based handgun shooting protocols (the adjusted size of target was chosen due to limited room dimension available in the research facility). Each trial was separated by 2 minutes (the order of AI and CON were randomized among the participants). For the testing, participants fired 10 shots, aiming to hit the middle of the circular target (a bullseye hit was worth 10 points, and 1 point was deducted for every 1 cm region away from the bullseye, resulting in a maximum score of 100 points). Participants were instructed to try to shoot as accurately as possible within a maximum time limit of 1-minute per trial. The sum of points from each trial was recorded for future analyses.
Overall, the paper is appropriately organized, well-written, and easy to follow. However, I do have many concerns, especially about the methods employed (familiarization, sleep control …), the study limitations (the sample size, blinding …), and the conclusions (repeating results …). I have listed these concerns in detail below.
2 We note that the grant information you provided in the ‘Funding Information’ and ‘Financial Disclosure’ sections do not match.
This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
There was also a statistically significant main effect of condition (F1, 18.142 = 10.576, pbonf = 0.005, η2 = 0.035), demonstrating that jump height after AI administration was higher (mean difference = 0.64 cm, pbonf = 0.005, Cohen’s d = 0.11 [0.03, 0.20]) compared to CON (Fig 6).
We appreciate your valuable feedback on improving the precision and focus of our discussion. Following your suggestion, we have thoroughly reviewed and rewritten the specified section to highlight the essential results regarding the impact of total sleep deprivation (TSD) and ammonia inhalants (AI) on performance tests. Unnecessary information, such as specific statistical details like 'condition × time interactions', has been removed to streamline the text and increase readability. In addition, to enhance consistency and navigability, we've added relevant subheadings - "Effect of Total Sleep Deprivation" and "Effects of Ammonia Inhalants".
The associated dataset and JASP outputs for all performed analyses are available at the Open Science Framework [OSF] repository (URL: https://osf.io/3rj84/; DOI 10.17605/OSF.IO/3RJ84).
Thank you for pointing out the potential inaccuracy in the sentence at line 724. We agree that the phrase "No matter the length of sleep deprivation" could be misinterpreted.
Due to the limited number of cadets at the Military department and the limited capacity of the sleep laboratory (6 participants per measurement at one time), the maximum number of participants was limited to 18. We performed sensitivity analyses to observed effects in our tests using G*Power (version 3.1.). For the within-factor differences and within-between interaction in repeated measures ANOVAs with α = 0.05, β = 0.8, N = 18, 2 conditions, and 5 testing sessions, we reached a sensitivity to observe a Cohen’s f = 0.267, which corresponds to η2 = 0.066 (default values of correlation and sphericity of 0.5 and 1, respectively, were used).
In addition, the rating of perceived exertion (RPE) was recorded during the CMJ testing using a CR-10 scale to evaluate RPE scores after each set of CMJ [44]. RPE is a frequently used marker of exercise intensity typically used for monitoring during exercise tests to complement other intensity measures [45].
The revised conclusion now reads: "These results indicate potential applications of AI in specific military scenarios, regardless of the presence or the length of total sleep deprivation. Nevertheless, caution is warranted in generalizing these results, given the study's limitations, such as the small, all-male sample size. Future research in this field would benefit from including more diverse participant groups and employing a wider range of military-related performance tests. This would provide a more comprehensive understanding of AI's effects under conditions of sleep deprivation, informing its potential utility in various operational contexts." We believe these amendments respond effectively to your concerns and provide a more rounded conclusion. Your astute observations and guidance have significantly contributed to improving the quality of our manuscript.
Additionally, there was statistically significant main effect of percentage difference between AI and CON during the same time spans (F3. 61.833 = 8.776, pbonf < 0.001, η2 = 0.340), where we observed greater percentage difference at 0–15 than 30–45 (mean difference = 3.67%, pbonf = 0.012, Cohen’s d = 1.02 [0.18, 1.85]) and 45–60 (mean difference = 4.08%, pbonf = 0.005, Cohen’s d = 1.13 [0.27, 2.00]) (Fig 5).
(A) Mean simple reaction time and (B) number of incorrect trials without (CON, white) and with ammonia inhalants (AI, black). Data are presented as mean (circles) and error bars represent their 95% confidence interval (LL, UL) at baseline (0 h), after 12 (-12 h), 24 (-24 h) and 36 (-36 h) hours of total sleep deprivation followed by 8 (+8 h) hours of recovery sleep.
Thank you for pointing out the need for clarification in line 185. We revised the sentence to explicitly indicate that the summary measures are for age, height, and weight. The revised sentence is: “Eighteen healthy male military cadets (age = 24.1 ± 3.0 years, height = 181.5 ± 6.3 cm, weight = 79.3 ± 8.3 kg, 4.0 ± 0.9 total years of service, all measurements reported as mean ± SD) serving at the Military department of Charles University participated in this study.”
Thank you for your suggestion to relocate the familiarization information to the methods section. However, we believe it's important to keep this information in the current section. The test in question is a military-specific test with a particular rifle, which is not commonly done. Therefore, we wanted to emphasize the reliability of this unique test in its immediate context. The familiarization information demonstrates that participants were adequately prepared for this specialized procedure, which adds to the reliability of the results. We appreciate your understanding in this matter and value your thoughtful feedback.
One of the most widely used ergogenic aids consumed by military personnel is caffeine [24]. According to prior research, moderate doses of caffeine (approximately 200–300 milligrams) have been found to sustain cognitive functioning, such as alertness and attention [24, 25] or enhance physical performance [25] during sleep deprivation. However, the use of caffeine cannot serve as a replacement for regular sleep. Excessive caffeine consumption can further disrupt sleep patterns, particularly if consumed within six hours prior to bedtime [26, 27]. Furthermore, multiple reviews and meta-analyses [28] show the potential positive effects of caffeine are likely to manifest about 1 hour after ingestion relative to, which may not be sufficient if immediate assistance is required. Therefore, fast-acting forms of ergogenic aids could be beneficial in such circumstances.
This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
In the manuscript, we have outlined the familiarization process stating, "They then completed a series of questionnaires addressing psychological and physiological health, which were followed by a general familiarization of the layout of the facility (i.e., location of the bathrooms, testing stations, etc.). During this familiarization, the participants were also familiarized with the specific testing procedures and practiced each of the required tasks."
1. Style Requirements: We have thoroughly revised the manuscript to align with PLOS ONE’s style guidelines, utilizing the provided templates for both the main body and title, authors, and affiliations.
The presented study found that the mean countermovement jump (CMJ) height was higher among participants during the evenings as compared to all morning measurements (3.0–4.7%). The observed outcome aligns with the circadian rhythm reported in the preceding sections. Specifically, the pattern of results associated with total sleep deprivation adheres to expectations, whereas the morning session conducted after 24 h of total sleep deprivation (a point where participants were reported to be most tired based on ESS scores) does not yield worse results than those obtained after 0 h, and following 8 h of recovery sleep. Additionally, evening sessions conducted after 36 h of total sleep deprivation did not yield worse outcomes than those obtained after 12 h (Fig 5A) This finding can be attributed to the increased performance in the CMJ, which demonstrates a clear circadian rhythm, with superior outcomes recorded during the afternoon relative to the morning, as described in previous research studies [79, 80]. Total sleep deprivation has been suggested to affect short-term anaerobic performance, such as jumping, by reducing motivation [81] and increased mental fatigue [82]. However, this study did not collect any of such measures, leaving this interpretation of results as speculative.
Thank you for your suggestion to include the reference by Khcharem et al., 2020, in our manuscript. We appreciate your efforts in identifying this relevant piece of work which aligns with the context discussed on line 516. We have incorporated this reference into the stated section.
Disclaimer: The views expressed are solely those of the authors and do not reflect the official policy or position of the Czech Army, the Department of Defense, or the Czech Government.
(A) Mean rating of perceived exertion (RPE) without (CON, white) and with ammonia inhalants (AI, black). Data are presented as mean (circles) and error bars represent their 95% confidence interval (LL, UL) at baseline after a full night of sleep (0 h), after 12 (-12 h), 24 (-24 h) and 36 (-36 h) hours of total sleep deprivation followed by 8 (+8 h) hours of recovery sleep. (B) Mean Epworth Sleepiness Scale (ESS) score. Data are presented as mean (circles) and error bars represent their 95% confidence interval (LL, UL) at baseline after a full night of sleep (0 h), after 12 (-12 h), 24 (-24 h) and 36 (-36 h) hours of total sleep deprivation followed by 8 (+8 h) hours of recovery sleep.
Overall, despite the lack of reduction in the adverse effects of total sleep deprivation, the use of AI was found to cause a short-term increase in HR and enhance SRT without increasing the number of errors and increase CMJ height while concurrently decreasing the RPE. However, no changes were observed in handgun shooting accuracy and manual dexterity performance. These results indicate potential applications of AI in specific military scenarios, regardless of the presence or the length of total sleep deprivation. Nevertheless, caution is warranted in generalizing these results, given the study’s limitations, such as the small, all-male sample size. Future research in this field would benefit from including more diverse participant groups and employing a wider range of military-related performance tests. This would provide a more comprehensive understanding of AI’s effects under conditions of sleep deprivation, informing its potential utility in various operational contexts.
Overall, the paper is appropriately organized, well-written, and easy to follow. However, I do have many concerns, especially about the methods employed (familiarization, sleep control …), the study limitations (the sample size, blinding …), and the conclusions (repeating results …). I have listed these concerns in detail below.
6. PLOS authors have the option to publish the peer review history of their article (what does this mean?). If published, this will include your full peer review and any attached files.
Assuming that inhaling AIs could be associated with higher arousal [29], we had predicted that AI could attenuate the shooting accuracy decrements that would be caused by sleep deprivation [68]. However, in the context of the present study, neither sleep deprivation nor the presence of AI (i.e., increased HR) affected shooting accuracy. The results of our study partially concur with previous research that found that the live-fire shooting accuracy of trained soldiers was not impacted by total sleep deprivation ranging from 24 to 36 h [69, 70]. However, it has been reported that similarly extended total sleep deprivation resulted in impaired live-fire shooting accuracy among conventional military personnel and non-military trained individuals [15, 71, 72]. This possibly suggests that more experienced shooters (with longer training experience) may be more resilient to the possible adverse effects of total sleep deprivation, which may explain the consistent shoot accuracy found in the present study.
In response to your suggestion, we have revised this statement to provide a clearer, more precise assertion. The updated sentence now reads: "regardless of the presence or the length of total sleep deprivation." We appreciate your diligent attention to detail and your constructive feedback, which have been instrumental in improving the clarity and accuracy of our manuscript.
For example, prior research has documented an immediate increase in heart rate [31, 32] and a concurrent increase in middle cerebral artery blood flow velocity [31], following the inhalation of AI, indicating a transient cerebrovascular vasodilation effect that persisted for 15–30 seconds. Despite the absence of evidence indicating that AI inhalation has an impact on maximal muscular strength or endurance [29], some evidence suggests that AI may enhance alertness [32], perceived performance [32], explosive strength during isometric muscle actions [33], as well as repeated anaerobic power performance when athletes were already fatigued [34, 35]. However, no effects were observed in dynamic "real-world" movements such as jump height [32] or sprint time [29]. In addition to that, it is important to note that while AI are widely prevalent among strength-based athletes, there is currently a significant gap in the literature regarding their specific effects on cognitive and physical performance [29].
Acknowledging the potential risks of AI, it is crucial to mention that under certain conditions it can be toxic, potentially cause allergic reactions, mask concussive symptoms, and exacerbate breathing difficulties for those with respiratory issues. These risks emphasize that despite its common use for reviving fainting individuals in the U.S, the use of AI for enhancing athletic performance should be carried out under caution and professional supervision [29]. However, it is worth noting that we did not observe any adverse effects associated with its use during our research.
An unmarked version of your revised paper without tracked changes. You should upload this as a separate file labeled 'Manuscript'.
It is widely acknowledged that the autonomic nervous system influences heart rate (HR) through the discharges of the sympathetic and the parasympathetic nervous system via sympathetic and vagal innervations, respectively [62]. However, evidence regarding the effect of total sleep deprivation on these systems, remains inconsistent [62]. One study reported [63] that after 30 h of total sleep deprivation, there was a decrease in cardiac sympathetic activity, but no change in parasympathetic, which contradicts the findings of another study [64] that found increased sympathetic activity and decreased parasympathetic activity following 36 h of total sleep deprivation. Despite the inconsistent findings of previous studies, our results indicated that HR during shooting protocol was lower after 24 h of total sleep deprivation, with a slight increase after 36 h, without considering the effects of AI. These results partly align with the outcomes of laboratory studies that controlled for environmental and behavioral influences such as sleep, light and activity, reporting that 24–30 h of total sleep deprivation results in a decrease in HR in healthy young individuals [65–67]. This decline in HR is typically superimposed on a 24-h rhythm [63], which could be a potential explanation for the increase in HR after 36 h of sleep deprivation in the current study.
Statistical analyses were conducted using JASP (version 0.16.2, 2022) [47]. Parametric tests were performed once the normality assumptions were verified using the Shapiro-Wilk test. Data were analyzed using a two-way repeated measures ANOVA (2 conditions: [AI, CON] × 5 time: [0 h, -12 h, -24 h, -36 h, +8 h]). Heart rate values were analyzed using a three-way repeated measures ANOVA (2 conditions: [AI, CON] × 5 time: [0 h, -12 h, -24 h, -36 h, +8 h] × 4 time spans: [0–15, 15–30, 30–45, 45–60 sec]). Lastly, the heart rate percentage difference values were analyzed using a one-way repeated measures ANOVA (1 condition: [heart rate percentage difference between AI and CON] × 4 time spans: [0–15, 15–30, 30–45, 45–60 sec]). Sphericity was assessed using Mauchly’s W. In cases where sphericity assumptions were violated, a Greenhouse–Geisser adjustment was applied. When the ANOVA tests demonstrated a statistically significant condition × time (× time spans or × percentage difference) interaction or a statistically significant main effect for condition, time, time spans, or percentage difference, post-hoc comparisons of the mean differences were performed using the Bonferroni correction (pbonf). Non-significant interaction effects were excluded from the models prior to the examination of main effects. The variance explained by each ANOVA model is reported in η2, and the mean difference effect sizes are reported as Cohen’s d with 95% lower limit (LL) and upper limit (UL) confidence intervals [LL, UL].
We have updated the text to include the explanation for "LL" and "UL". The revised text now reads: "Cohen’s d with 95% lower limit (LL) and upper limit (UL) confidence intervals [LL, UL]." Your attention to detail is greatly appreciated and contributes to the overall clarity of the manuscript.
We believe these revisions address your concerns effectively, ensuring a focused and concise discussion section. We are grateful for your guidance and continued assistance in refining our manuscript.
(A) Mean heart rate (bpm) without (CON, white) and with ammonia inhalants (AI, black). Data are presented as mean (circles) and error bars represent their 95% confidence interval (LL, UL) at baseline (0 h), after 12 (-12 h), 24 (-24 h) and 36 (-36 h) hours of total sleep deprivation followed by 8 (+8 h) hours of recovery sleep. (B) Mean heart rate (bpm) without (CON, white) and with ammonia inhalants (AI, black). Data are presented as mean (circles) and error bars represent their 95% confidence interval (LL, UL) as an average of 15-second time spans (0–15, 15–30, 30–45, and 45–60) during shooting trials regardless of sleep deprivation.
3. Please include your tables as part of your main manuscript and remove the individual files. Please note that supplementary tables (should remain/ be uploaded) as separate "supporting information" files.
Do you want your identity to be public for this peer review? For information about this choice, including consent withdrawal, please see our Privacy Policy.
- I suggest that this section should be rewritten in a more precise way. It should focus on essential results about the main subject: the impact of TSD on the tests selected, and the impact of AI on performance tests (by describing the scientific reasons about previous similar works, without repeating results or useless information).
-L213-217: The experimental protocol was not blinded in this study. This latter could influence the performance outcomes (participants could be more motivated with AI supplement) which could limit the study conclusions. This should be added in the section of the study limitations.
4- Results: For clarity, state that non-significant interaction effects were dropped from the models before testing main effects. Tables of these results would help readers better grasp the them.
-L173: As outlined before, “cadets” need to be explained in parentheses (“young armed”, “police force”) to be clearer for readers.
Thank you very much for your suggestion regarding the "short-term increase in HR" in our conclusion. We understand your point about focusing on key performance outcomes related to the impact of AI during TSD. However, we have decided to retain this information in our conclusion due to its importance in drawing parallels to previous studies on the same topic. We believe mentioning all relevant variables in the conclusion will ensure comprehensiveness and transparency allowing for a holistic understanding of the results.
Sleep is a fundamental yet often undervalued physiological process, indispensable for maintaining physical and mental well-being [1]. It is an essential component of our circadian rhythms, which have been found to profoundly influence both cognitive and physical performance [2]. However, these rhythms can easily be disrupted due to various factors such as stress, jetlag, travelling, or night-shift work. Such disruptions can result in cognitive and physical deficits, poorer mental health, and elevated health risks [3, 4]. Therefore, a deeper insight into the relationships between disruption to sleep and their combined effect on cognitive and physical performance is of paramount importance. This knowledge, while vital for all, may be especially critical for at-risk occupations such as military personnel. It has the potential to significantly influence their health and combat readiness [5]. Given this, the optimization of health, well-being, and overall performance could be particularly crucial for them [6, 7]. The necessity of maintaining adequate sleep quality and quantity thus becomes evident, underscoring the integral role sleep plays in the well-being and performance of military personnel.
We are deeply appreciative of the insightful comments provided on our manuscript. The reviewers' constructive feedback was instrumental, guiding us in refining and enhancing our work. After incorporating these suggestions, we believe the manuscript has become significantly stronger, more comprehensive, and better positioned to contribute meaningfully to the field.
Thank you also for suggesting the inclusion of tables to enhance readers' understanding of the results. While we acknowledge the value this would add, we have chosen to include all detailed tables in the supplementary materials available online. This approach allows interested readers to access all the specifics while maintaining the conciseness of the manuscript.
We appreciate your observation on the lack of blinding in our study and the potential influence it could have on the performance outcomes. Indeed, the distinct smell and immediate physical response after inhalation of ammonia inhalants (AIs) render a true placebo control virtually impossible. In response to your suggestion, we have added the following to the limitations section of our manuscript: "Additionally, one limitation of this study was the absence of a placebo condition due to the distinct characteristics of AIs. Participants can likely distinguish AIs from any potential placebo due to their strong smell and immediate physical response after inhalation. Though some placebo substances like menthol oil or Vicks VapoRub have been used in other studies, these also have identifiable smells that can potentially compromise the blinding process. Consequently, participants in our study likely knew when they were not inhaling an AI. Nonetheless, no studies have reported an increase in performance superior to AI inhalation for placebo or control conditions, indicating a limited placebo effect in this context." We believe this paragraph effectively addresses the limitation you highlighted, and we appreciate your thoughtful suggestion.
- L104: I suppose that there is a lack of general introduction concerning the disrupted sleep-wake cycle in everyday life (stress, shift work, jetlag…) before moving on to the part that specifies its relation with the military.
The manuscript has been evaluated by one reviewer and a member of our statistical advisory board, and their comments are available below. They have raised a number of concerns that need attention. They request additional information on methodological aspects of the study, revisions to the statistical analyses and revisions to the Discussion to ensure that the conclusions are presented appropriately.
Please submit your revised manuscript by Aug 19 2023 11:59PM. If you will need more time than this to complete your revisions, please reply to this message or contact the journal office at plosone@plos.org. When you're ready to submit your revision, log on to https://www.editorialmanager.com/pone/ and select the 'Submissions Needing Revision' folder to locate your manuscript file.
-L173: As outlined before, “cadets” need to be explained in parentheses (“young armed”, “police force”) to be clearer for readers.
In cases where the interaction effects were non-significant, we have removed them from the model and focused on testing the main effects as recommended.
[NOTE: If reviewer comments were submitted as an attachment file, they will be attached to this email and accessible via the submission site. Please log into your account, locate the manuscript record, and check for the action link "View Attachments". If this link does not appear, there are no attachment files.]
If applicable, we recommend that you deposit your laboratory protocols in protocols.io to enhance the reproducibility of your results. Protocols.io assigns your protocol its own identifier (DOI) so that it can be cited independently in the future. For instructions see: https://journals.plos.org/plosone/s/submission-guidelines#loc-laboratory-protocols. Additionally, PLOS ONE offers an option for publishing peer-reviewed Lab Protocol articles, which describe protocols hosted on protocols.io. Read more information on sharing protocols at https://plos.org/protocols?utm_medium=editorial-email&utm_source=authorletters&utm_campaign=protocols.
-L163: I wonder if there are negative effects of AI in the literature (you should report in addition to the test results if there are any observed negative effects (during the experiments) of this stimulant in the discussion section).
There was faster SRT (1.6%; p < 0.01) without increasing the number of errors, higher JH (1.5%; p < 0.01), lower RPE (9.4%; p < 0.001), and higher HR (5.0%; p < 0.001) after using AI compared to CON regardless of TSD. However, neither SA nor DAS were affected by AI or TSD (p > 0.05). Independent of AI, the SRT was slower (3.2–9.3%; p < 0.001) in the mornings (-24, +8) than in the evening (-12), JH was higher (3.0–4.7%, p < 0.001) in the evenings (-12, -36) than in the mornings (0, -24, +8), and RPE was higher (20.0–40.1%; p < 0.001) in the sleep-deprived morning (-24) than all other timepoints (0, -12, -36, +8). Furthermore, higher ESS (59.5–193.4%; p < 0.001) was reported at -24 and -36 than the rest of the time points (0, -12, and + 8).
Based on previous studies [20, 83], total sleep deprivation may also lead to changes in the perception of effort. The RPE increased after 24 to 30 h of total sleep deprivation alongside a decrease in performance [20, 83]. These previous observations partly align with the results of the present study, where the highest RPE was reported after 24 h of total sleep deprivation (Fig 7A), which also corresponded with the highest level of subjective sleepiness reported by our participants (Fig 7B). Although our participants reported feeling less tired at 36 h than after 24 h (28.6%) of total sleep deprivation, this apparent "improvement" should not be interpreted as an actual improvement, but it is rather a continuation of the circadian rhythm. Eventually, the night of recovery sleep seemed to more or less returned the perception of sleepiness to levels in line with the 0 h of total sleep deprivation and normal circadian rhythm.
In our manuscript, we have expanded discussion part upon these points, using the following text: “Acknowledging the potential risks of AI, it is crucial to mention that it can be toxic under certain conditions, potentially cause allergic reactions, mask concussive symptoms in contact sports, and exacerbate breathing difficulties for those with respiratory issues. These risks emphasize that despite its legality in the U.S. for reviving fainting individuals, the use of AI for enhancing athletic performance should be carried out under caution and professional supervision (29). However, it is worth noting that we did not observe any adverse effects associated with its use during our research.”
Participants reported to the Sleep and Chronobiology laboratory (National Institute of Mental Health) on Thursday evening after a standardized dinner at ~18:00 h. They then completed a series of questionnaires addressing psychological and physiological health, which were followed by a general familiarization of the layout of the facility (i.e., location of the bathrooms, testing stations, etc.). During this familiarization, the participants were also familiarized with the specific testing procedures and practiced each of the required tasks.
This paper investigated the effect of ammonia inhalants (i.e. a fast-acting ergogenic aid) on cognitive and physical performance (i.e. 5 tests repeated in 5-time points) during a night of total sleep deprivation (i.e. 36 hours of sleep deprivation) in young military personnel (i.e. 18 male cadets).
Although healthy adults need an average of 7.5 to 8.5 hours of sleep per day [8, 9], self-reported data indicates that military personnel in various branches of service obtain less sleep [10], which may have a detrimental effect on the ability to perform military duties efficiently [11]. Furthermore, a considerable proportion of military personnel is confronted with scenarios where they are required to carry out tasks incessantly and for up to 24 hours [12]. In situations of military operational necessities such as overnight duty, prolonged operations, or direct ground combat, some soldiers may endure a lack of sleep that can surpass 24 hours, a condition known as total sleep deprivation [13]. Research suggests that total sleep deprivation can decrease blood flow velocity in the middle cerebral artery [14], a major blood vessel that supplies the brain with oxygenated blood. This decrement has been shown to contribute to various physical, cognitive and behavioral impairments, such as fatigue and impaired sustained attention and reaction time [14]. Moreover, extant research has indicated that manual dexterity, a critical component of tasks like shooting and firearms handling, may be negatively impacted by total sleep deprivation. Previous investigations have reported that the absence of sleep for a period from 24 to 72 hours can lead to a reduction in shooting accuracy, ranging from 13% to 37% [15, 16] Additionally, another study [17] has demonstrated that even a single night of total sleep deprivation may have deleterious effects on manual dexterity and hand-eye coordination, resulting in a decrease in performance by 32%.
In line with your feedback, we have revised the text as follows: "Sleep is a fundamental yet often undervalued physiological process, indispensable for maintaining physical and mental well-being (1). It is an essential component of our circadian rhythms, which have been found to profoundly influence both cognitive and physical performance (2). However, these rhythms can easily be disrupted due to various factors such as stress, jetlag, travelling, or night-shift work. Such disruptions can result in cognitive and physical deficits, poorer mental health, and elevated health risks (3,4).” We believe this change provides a clearer and more comprehensive definition of sleep, enhancing the understanding of our manuscript. Thank you for your constructive feedback.
I suggest that the conclusion needs to be reformulated; there is no need to repeat the results in this section and with the same abbreviations, (e.g. ammonia inhalant markedly improved the reaction time, jumping, and sensation of pain of soldiers). It should conclude the main results in a good manner. In addition, it should be tempered (e.g. in similar testing conditions of prolonged sleep deprivation). It should also finish with a recommendation for future studies about this topic (e.g., Further investigations including females and using different tests are needed…)
Thank you for your question about the duration effect of ammonia inhalants (AI). While it is indeed an important factor, to our best knowledge and as described in our previously published review (DOI: 10.1519/SSC.0000000000000630), no research has specifically reported the half-life of ammonia inhalants. However, it has been noted that AIs likely produce significant cerebrovascular, cardiovascular, and respiratory responses 7.5–15 seconds after inhalation (possibly up to under 30 seconds), but then these variables return to baseline values after 30 seconds. As such, it appears that the timing of inhalation before performance may be one of the most significant conditions when using AIs as an ergogenic aid.
An example of a fast-acting ergogenic aid are ammonia inhalants (AI), which are commonly used as a fast-acting "pre-workout stimulant", whereby users hope for rapid improvements in vigilance and short-term high-intensity physical performance [29]. The putative effect of arousal via AI inhalation is believed to be caused by irritation of the respiratory passages that may subsequently trigger the adrenergic receptors in peripheral tissue, resulting in the release of norepinephrine, causing an increase in cardiac output, respiratory rate [30] and an increase in blood flow velocity in the middle cerebral artery [31].
We appreciate your attention to the potential negative effects of Ammonia Inhalants (AI). We have indeed considered this crucial aspect and included it in our discussion. To briefly summarize, exposure to large doses of concentrated ammonia vapors can result in injuries such as allergic reactions, respiratory airway burns, and distress, among others. Furthermore, although commercially available AI capsules release significantly lower amounts of ammonia vapors, some potential risks remain, including allergic reactions requiring medical attention, possible masking of head injury symptoms in contact sports, and potential respiratory difficulties in individuals with existing respiratory problems.
If you would like to make changes to your financial disclosure, please include your updated statement in your cover letter. Guidelines for resubmitting your figure files are available below the reviewer comments at the end of this letter.
Please submit your revised manuscript by Oct 30 2023 11:59PM. If you will need more time than this to complete your revisions, please reply to this message or contact the journal office at plosone@plos.org. When you're ready to submit your revision, log on to https://www.editorialmanager.com/pone/ and select the 'Submissions Needing Revision' folder to locate your manuscript file.
3. Please include your tables as part of your main manuscript and remove the individual files. Please note that supplementary tables (should remain/ be uploaded) as separate "supporting information" files.
There was also statistically significant main effect of condition (F1, 3.472 = 17.220, pbonf < 0.001, η2 = 0.034), demonstrating that soldiers reported higher RPE at CON compared to after usage of AI (mean difference = 0.28, pbonf < 0.001, Cohen’s d = 0.30 [0.11, 0.48]) (Fig 7A).
-L163: I wonder if there are negative effects of AI in the literature (you should report in addition to the test results if there are any observed negative effects (during the experiments) of this stimulant in the discussion section).
By maintaining the term "condition," we ensure consistency and clarity throughout the manuscript, allowing readers to easily follow and understand the experimental setup. We value your feedback and always strive to enhance the clarity of our work.
In our study, the term "condition" refers to the experimental conditions being compared, specifically the ammonia inhalant condition and the control condition. Using the term "ammonia" instead of "condition" may potentially create confusion for readers who are unfamiliar with the study design or the specific terminology used in the field.
Even though SRT was slower in the mornings as compared to the evenings, our study aimed to determine whether using AI would affect SRT during total sleep deprivation. Partly in line with our predictions, SRT was faster following the use of AI (1.6%), but AI had no greater effect on SRT during sleep deprivation than when fully rested. Regardless of sleep deprivation, these ergogenic effects of AI are thought to be mediated by the activation of the olfactory and trigeminal nerves, which leads to the activation of the adrenergic receptor and the subsequent release of norepinephrine, resulting in an increase in cardiac output and respiratory rate [29]. This effect has been shown to result in an increase in beat-to-beat middle cerebral artery blood flow velocity [31], which may be linked to enhanced cognitive performance [57].
In simple reaction times, we observed statistically significant main effect of time (F2.30, 6291.19 = 4.99, p = 0.009, η2 = 0.19, with Greenhouse-Geisser correction). In subsequent post-hoc comparisons, the simple reaction time was statistically significantly slower at -12 compared to -24 (mean difference = 26.74 ms, pbonf = 0.002, Cohen’s d = 1.05 [0.15, 1.94]) and + 8 (mean difference = -18.04 ms, pbonf = 0.007, Cohen’s d = 0.70 [-1.51, -0.10]) (Fig 3A).
- Line 79 (also Line 173): I suggest replacing “cadets” because it is with double meaning, or explaining it in parentheses (“young armed”, “police force”) to avoid confusion.
Official websites use .gov A .gov website belongs to an official government organization in the United States.
This study aimed to investigate the potential effect of AI usage on simple reaction time, shooting accuracy, countermovement jump height, and rifle disassembly and reassembly time during 36 h of total sleep deprivation, followed by 8 h of recovery sleep in military personnel. The principal findings of our investigation were that although both total sleep deprivation and AI affected some variables during the study protocol, AI inhalation did not have a great effect specifically during the period of sleep deprivation. Nevertheless, regardless of sleep deprivation, AI use increased heart rate from 0–15 seconds after inhalation, improved simple reaction time without increasing the number of errors, and increased countermovement jump height while simultaneously decreasing rating of perceived exertion. No changes in shooting accuracy or the rifle disassembly and reassembly time after AI were observed.
-L184: The participants' sleep quality (and quantity) is a very important measurement for such a study. For example, the sleep quality of athletes could be determined using the questionnaire of Horne and Östberg (1976). This latter could inform about the participants rising times, bedtimes, and sleep disorders.
This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Thank you for your suggestion to reformulate our sentence on lines 116 and 117. We have added "physical" to the sentence as per your recommendation. However, regarding your suggestion to change "impaired" to "decreased", we have decided to retain the term "impaired". We believe that "impaired" offers a more comprehensive understanding, indicating not only a potential decrease in attention and reaction time, but also the possibility of increased errors.
-L516: This reference is important and could also be added; Amir Khcharem, Makram Souissi, Rim Atheymen, Lobna Ben Mahmoud & Zouheir Sahnoun (2020): Effects of caffeine ingestion on 8-km run performance and cognitive function after 26 hours of sleep deprivation, Biological Rhythm Research, DOI: 10.1080/09291016.2020.1778975
If applicable, we recommend that you deposit your laboratory protocols in protocols.io to enhance the reproducibility of your results. Protocols.io assigns your protocol its own identifier (DOI) so that it can be cited independently in the future. For instructions see: https://journals.plos.org/plosone/s/submission-guidelines#loc-laboratory-protocols. Additionally, PLOS ONE offers an option for publishing peer-reviewed Lab Protocol articles, which describe protocols hosted on protocols.io. Read more information on sharing protocols at https://plos.org/protocols?utm_medium=editorial-email&utm_source=authorletters&utm_campaign=protocols.
-L156: I suppose that the duration effect is also an important thing. Is there any information about how long it last for AI (the half-life of caffeine lasts between 2.5 and 4.5 h in humans)?
PONE-D-23-07437Effects of 36 hours of sleep deprivation on military-related tasks: can ammonium inhalants maintain performance?PLOS ONE
Thank you for your suggestions regarding the selection of keywords. We have adopted your recommendations of replacing "tests" with "Performance" and keeping "Army" while removing "Soldiers". However, we have chosen to retain "Ergogenic Aids" and "sleep loss" as they are broader terms that encapsulate "Ammonia Inhalants" and "Sleep Deprivation", respectively, which are already included in main tittle of manuscript. These keywords also align with the title of our manuscript and we believe it will aid in its visibility and reach.
Nevertheless, this study also investigated the impact of AI inhalation on HR during shooting protocol while total sleep deprived. Our findings are in line with a previous study [31], which demonstrated that AI elicits a strong cardiovascular response that results in an elevation of HR compared to control trials without AI. Additionally, our results showed that this response was observed immediately after AI inhalation, with HR increasing in the first 15 seconds (7.3% compare to CON) and then gradually declining (Fig 5). That is consistent with prior reports indicating that the effect of AI on the cardiovascular system is typically short-term and may not provide a sustained ergogenic benefit beyond the initial 15 seconds of inhalation [29, 31].
If the interaction effect is significant, provide an interpretation of the results, but do not test main effects because the tests for main effects are uninteresting in light of significant interactions. If interaction effects are non-significant, drop the interaction effects from the model and test the main effects. Determining which results to present when testing interactions is often a multi-step process. Typically these type of results are presented in table format because they are more easily comprehendable.
Hence, it is plausible that the increase in alertness following the use of AI may be attributed to improved delivery of oxygenated blood to the brain [58]. Previous studies have indicated that decreased cerebral blood flow can impair cognitive function [59], which may result in reduced arousal levels, ultimately leading to decreased performance [60]. Considering this evidence, the enhancement of alertness [32, 35] resulting from AI use may explain the widespread use of this stimulant. Nevertheless, it should be noted that the implications of these findings are beyond the scope of this study.
Data are presented as mean (circles) and error bars represent their 95% confidence interval (LL, UL) at the average of 15-second time spans (0–15, 15–30, 30–45, and 45–60) during shooting trials regardless of sleep deprivation.
The PLOS Data policy requires authors to make all data underlying the findings described in their manuscript fully available without restriction, with rare exception (please refer to the Data Availability Statement in the manuscript PDF file). The data should be provided as part of the manuscript or its supporting information, or deposited to a public repository. For example, in addition to summary statistics, the data points behind means, medians and variance measures should be available. If there are restrictions on publicly sharing data—e.g. participant privacy or use of data from a third party—those must be specified.
-L156: I suppose that the duration effect is also an important thing. Is there any information about how long it last for AI (the half-life of caffeine lasts between 2.5 and 4.5 h in humans)?
-L139: I suppose that this study is very interesting about this topic and it could be added as a recent reference (Repeated low-dose caffeine ingestion during a night of total sleep deprivation improves endurance performance and cognitive function in young recreational runners: A randomized, double-blind, placebo-controlled study (2022)
A marked-up copy of your manuscript that highlights changes made to the original version. You should upload this as a separate file labeled 'Revised Manuscript with Track Changes'.
Thank you for submitting your manuscript to PLOS ONE. After careful consideration, we feel that it has merit but does not fully meet PLOS ONE’s publication criteria as it currently stands. Therefore, we invite you to submit a revised version of the manuscript that addresses the points raised during the review process.
While revising your submission, please upload your figure files to the Preflight Analysis and Conversion Engine (PACE) digital diagnostic tool, https://pacev2.apexcovantage.com/. PACE helps ensure that figures meet PLOS requirements. To use PACE, you must first register as a user. Registration is free. Then, login and navigate to the UPLOAD tab, where you will find detailed instructions on how to use the tool. If you encounter any issues or have any questions when using PACE, please email PLOS at figures@plos.org. Please note that Supporting Information files do not need this step.
We observed statistically significant main effect of time (F4, 2959.875 = 8.515, pbonf < 0.001, η2 = 0.126) on heart rate during shooting. In subsequent post-hoc tests, the heart rate was statistically significantly slower at 0 than at -12 (mean difference = 9.29 bpm, pbonf = 0.004, Cohen’s d = 0.84 [0.15, 1.53]) and also slower at -24 compare to -12 (9.75 bpm, pbonf = 0.001, Cohen’s d = 0.88 [0.17, 1.59]) and -36 (5.63 bpm, pbonf = 0.018, Cohen’s d = 0.51 [0.09, 1.11]) (Fig 4A).
An unmarked version of your revised paper without tracked changes. You should upload this as a separate file labeled 'Manuscript'.
4- Results: For clarity, state that non-significant interaction effects were dropped from the models before testing main effects. Tables of these results would help readers better grasp the them.
-L143: “The potential positive effects of caffeine are likely to manifest about 1 hour after ingestion relative to many reviews and meta-analysis (and not between 10 and 60 min) (Reference: Grgic J, Grgic I, Pickering C, et al. Br J Sports Med 2020;54:681–688)
Please note that we have only been able to secure a single subject reviewer to assess your manuscript. We are issuing a decision on your manuscript at this point to prevent further delays in the evaluation of your manuscript. Please be aware that the editor who handles your revised manuscript might find it necessary to invite additional reviewers to assess this work once the revised manuscript is submitted. However, we will aim to proceed on the basis of this single review if possible.
When you resubmit, please ensure that you provide the correct grant numbers for the awards you received for your study in the ‘Funding Information’ section.
7. PLOS authors have the option to publish the peer review history of their article (what does this mean?). If published, this will include your full peer review and any attached files.
The manuscript must describe a technically sound piece of scientific research with data that supports the conclusions. Experiments must have been conducted rigorously, with appropriate controls, replication, and sample sizes. The conclusions must be drawn appropriately based on the data presented.
-L196: Is there a familiarization (before the testing day) with the sleep deprivation (36 hours) to be familiar with the experimental process and the sleep adaptation? If yes, describe this familiarization.
In addition to the detrimental effects on cognitive functioning and perceptual-motor skills, research has demonstrated that total sleep deprivation also impairs short-term, high-intensity exercise output. Previous research has demonstrated that total sleep deprivation lasting for 24 hours can lead to a reduction of 2% to 10% in 15-meter sprint speed [18–20] and exhaustive time on 400-meter run by 10% [21]. Moreover, after 36 hours of total sleep deprivation, short-term maximal anaerobic performance has been reported to decrease by 5% [22]. Given that soldiers frequently need to perform intense, short-term movements such as sprinting across a battlefield or traversing obstacles in various terrain conditions, a decline in this type of performance may negatively impact a soldier’s survival and effectiveness in combat. Since the potential risks and high-stakes nature of military service, the detrimental effects of impaired sleep on cognitive and physical functioning are of significant concern. As such, ergogenic aids, which can alleviate these negative effects by promoting alertness and augmenting physical performance, are of interest to military [23].
-L202: How to be sure that participants have really passed 8 hours of recovery sleep? In the same context; how to be sure that the circadian rest-activity rhythms of the 18 subjects included in the study are well synchronized? It is obvious that only the use of devices for recording activity (actimeter, polysomnograph) or temperature, which are considered marker rhythms, could confirm the synchronization. Unfortunately, this was not carried out in this study.
-L390-443: There is no need to present all the results especially when they are unnecessary (or not important for the conclusions) and will bother readers.
Reviewer #2: A single cohort study of 18 healthy male cadets investigated the acute effects of ammonia inhalants (AI) versus control on cognitive and physical performance during a 36 hour period of total sleep deprivation (TSD). ANOVA methods were used to analyze the main objectives of the trial. The conclusions are unclear.
- L101, 102: The conclusion should be tempered and corrected; “AI could considerably improve performance in similar conditions and tests regardless of TSD (and not any duration of SD)”
Thank you for your insightful comment regarding the use of the term "cadets". We have added the word "military" before "cadets" throughout the manuscript.
We hope that these revisions address your concerns adequately. We are grateful for your expert review, as it has significantly contributed to improving the rigor and clarity of our manuscript.
-L192: I suppose that the time should be written in a scientific article: 18:00 h and not in the military version: 1800 h (to be replaced throughout the manuscript)
Thank you for this comment. We appreciate your concern about the confirmation of sleep duration and synchronization of circadian rhythms. Indeed, to ensure the accuracy of our study, we had the participants wear actigraphs throughout the duration of the experiment, and they also underwent polysomnography during their recovery sleep. Polysomnography EEG activities were scored according to international criteria [Iber, C. (2007). The AASM manual for the scoring of sleep and associated events: rules, terminology, and technical specification] by trained evaluators. On average, the participants achieved 8 hours and 28 minutes of recovery sleep (+/- 11 minutes) from polysomnography testing and 7 hours and 45 minutes (+/- 30 minutes) from actigraphs testing from Saturday to Sunday.
-L319-323: The familiarization information should be written in the methods section. In this section, we only describe the realization of the test.
If the interaction effect is significant, provide an interpretation of the results, but do not test main effects because the tests for main effects are uninteresting in light of significant interactions. If interaction effects are non-significant, drop the interaction effects from the model and test the main effects. Determining which results to present when testing interactions is often a multi-step process. Typically these type of results are presented in table format because they are more easily comprehendable.
Regarding your recommendation on how to handle and present interaction effects and main effects in the ANOVA analyses, we acknowledge the importance of correctly interpreting and reporting these effects. Following your guidance, we have adopted the multi-step process for presenting results when testing interactions:
Please use the space provided to explain your answers to the questions above. You may also include additional comments for the author, including concerns about dual publication, research ethics, or publication ethics. (Please upload your review as an attachment if it exceeds 20,000 characters)
-L258: I suggest starting by giving the quality measured by the test (accuracy, speed, strength) and the type of test (cognitive, physical, psychological), before the description, and this for all 5 tests (for more clarity).
Though there was no statistically significant main effect of time (F2.262, 2.619 = 1.437, pbonf = 0.250, η2 = 0.051, with Greenhouse-Geisser correction) for incorrect trials execution, there was statistically significant main effect of condition (F1, 3.200 = 6.800, pbonf = 0.018, η2 = 0.028), demonstrating that using AI reduced the amount of incorrect trials (mean difference = 0.267, pbonf = 0.018, Cohen’s d = 0.267 [0.04, 0.50]) (Fig 3B).
If you would like to make changes to your financial disclosure, please include your updated statement in your cover letter. Guidelines for resubmitting your figure files are available below the reviewer comments at the end of this letter.
Therefore this study aims to examine the effectiveness of AI in countering the effects of total sleep deprivation on cognitive and physical performance tests relevant to military personnel. We predict that soldiers will experience decreased cognitive and physical performance with prolonged total sleep deprivation. However, it is expected that the utilization of AI may mitigate these negative effects.
-L202: How to be sure that participants have really passed 8 hours of recovery sleep? In the same context; how to be sure that the circadian rest-activity rhythms of the 18 subjects included in the study are well synchronized? It is obvious that only the use of devices for recording activity (actimeter, polysomnograph) or temperature, which are considered marker rhythms, could confirm the synchronization. Unfortunately, this was not carried out in this study.
1. If the authors have adequately addressed your comments raised in a previous round of review and you feel that this manuscript is now acceptable for publication, you may indicate that here to bypass the “Comments to the Author” section, enter your conflict of interest statement in the “Confidential to Editor” section, and submit your "Accept" recommendation.
PLOS ONE does not copyedit accepted manuscripts, so the language in submitted articles must be clear, correct, and unambiguous. Any typographical or grammatical errors should be corrected at revision, so please note any specific errors here.
Additionally, ESS was also statistically significantly greater at -36 compared to 0 (mean difference = 7.78, pbonf < 0.001, Cohen’s d = 1.93 [0.63, 3.20]), -12 (mean difference = 5.17, pbonf = 0.002, Cohen’s d = 1.28 [0.25, 2.32]), and +8 (mean difference = 6.94, pbonf < 0.001, Cohen’s d = 1.72 [0.54, 2.91]) (Fig 7B).
Additionally, all participants wore a chest strap heart rate monitor (Polar Electro Inc., Model H10, Lake Success, NY, USA) during the shooting protocol. Baseline heart rate data were derived as a mean of heart rate from 2 minutes immediately preceding the start of the shooting trial. Heart rate (bpm) was then continuously monitored during all sessions of shooting protocol. After baseline testing, heart rate data were averaged in 15 seconds bins (0–15, 15–30, 30–45, 45–60) for one minute immediately following the AI and CON trials. The mean of these bins from each trial was used in subsequent analysis [31].
Thank you for your suggestion to clarify the handling of non-significant interaction effects in our analysis. We have added the sentence "Non-significant interaction effects were excluded from the models prior to the examination of main effects." to the Results section (at line 350), to address this point. We believe this addition will enhance the clarity of our methodology.
-L390-443: There is no need to present all the results especially when they are unnecessary (or not important for the conclusions) and will bother readers.
Please use the space provided to explain your answers to the questions above. You may also include additional comments for the author, including concerns about dual publication, research ethics, or publication ethics. (Please upload your review as an attachment if it exceeds 20,000 characters)
However, for ease of reporting and interpretation, we approximated this time to 8 hours in the manuscript. We understand your interest in the detailed data of sleep duration and quality, as well as circadian rhythms. However, these data are being used in a separate, larger-scale research paper that we are currently preparing for submission. We believe that this approach prevents the duplication of results across our publications. We hope this clarifies our decision for the methodology of this study.
Reviewer #1: The revision of the manuscript is satisfactory and the authors have addressed all the questions raised by the reviewers.
- L101, 102: The conclusion should be tempered and corrected; “AI could considerably improve performance in similar conditions and tests regardless of TSD (and not any duration of SD)”
- L103: keywords are not well selected; I suggest adding Performance (not tests), Ammonia Inhalants (not Ergogenic Aids), Soldiers or Army (not both), and Sleep Deprivation (not sleep loss).
I'm pleased to inform you that your manuscript has been deemed suitable for publication in PLOS ONE. Congratulations! Your manuscript is now with our production department.
-L184: The participants' sleep quality (and quantity) is a very important measurement for such a study. For example, the sleep quality of athletes could be determined using the questionnaire of Horne and Östberg (1976). This latter could inform about the participants rising times, bedtimes, and sleep disorders.
One potential explanation may be that cognitive performance is influenced by the interplay between the sleep homeostatic system (i.e., the biological drive for sleep) and the circadian rhythm (i.e., synchronization with the 24-h day/night cycle) [52]. These systems operate in a coordinated manner, following a 24-h sinusoidal pattern, with increased or decreased levels of fatigue depending on the time of day. As a result, total sleep deprivation can affect cognitive performance in a non-linear fashion, with the most pronounced cognitive impairments observed during the morning hours [53, 54]. Our results also align with previous research [55], where faster SRT was reported in the evenings (after 8–12 and 32–36 h of total sleep deprivation) compared to the morning (after 24 h of total sleep deprivation). This phenomenon is also known as the "wake maintenance zone", where the desire to sleep is usually the lowest in the evenings (2 to 3 h before the start of the melatonin secretion), and it is also maintained despite the increasing drive for sleep that results from total sleep deprivation [56].
-L213-217: The experimental protocol was not blinded in this study. This latter could influence the performance outcomes (participants could be more motivated with AI supplement) which could limit the study conclusions. This should be added in the section of the study limitations.
1. Please ensure that your manuscript meets PLOS ONE's style requirements, including those for file naming. The PLOS ONE style templates can be found at
-L192: I suppose that the time should be written in a scientific article: 18:00 h and not in the military version: 1800 h (to be replaced throughout the manuscript)
This paper investigated the effect of ammonia inhalants (i.e. a fast-acting ergogenic aid) on cognitive and physical performance (i.e. 5 tests repeated in 5-time points) during a night of total sleep deprivation (i.e. 36 hours of sleep deprivation) in young military personnel (i.e. 18 male cadets).
-L516: This reference is important and could also be added; Amir Khcharem, Makram Souissi, Rim Atheymen, Lobna Ben Mahmoud & Zouheir Sahnoun (2020): Effects of caffeine ingestion on 8-km run performance and cognitive function after 26 hours of sleep deprivation, Biological Rhythm Research, DOI: 10.1080/09291016.2020.1778975
1. If the authors have adequately addressed your comments raised in a previous round of review and you feel that this manuscript is now acceptable for publication, you may indicate that here to bypass the “Comments to the Author” section, enter your conflict of interest statement in the “Confidential to Editor” section, and submit your "Accept" recommendation.
2. Funding Information: We apologize for the discrepancy in the grant information. This has been corrected to accurately reflect the grant numbers in the 'Funding Information' section.
During the testing protocol, data were recorded for 14 of the 18 participants. The remaining four participants were unable to participate in the familiarization due to service duties and were thus excluded from the respective subsequent analysis.
PLOS ONE does not copyedit accepted manuscripts, so the language in submitted articles must be clear, correct, and unambiguous. Any typographical or grammatical errors should be corrected at revision, so please note any specific errors here.
While revising your submission, please upload your figure files to the Preflight Analysis and Conversion Engine (PACE) digital diagnostic tool, https://pacev2.apexcovantage.com/. PACE helps ensure that figures meet PLOS requirements. To use PACE, you must first register as a user. Registration is free. Then, login and navigate to the UPLOAD tab, where you will find detailed instructions on how to use the tool. If you encounter any issues or have any questions when using PACE, please email PLOS at figures@plos.org. Please note that Supporting Information files do not need this step.
For the post-hoc comparisons, we calculated the sensitivity for two-tailed t-tests of dependent means with matched pairs. With a Bonferroni-adjusted α of 0.01 (calculated as 0.05 divided by the number of comparisons, 5 in our case), β = 0.8 [48], N = 18, we reach sensitivity to observe an effect size (Cohen’s d) of 0.894.
It has been documented that prolonged periods of total sleep deprivation can impair sustained vigilance, which may negatively impact cognitive performance [49, 50] and potentially impair military readiness. The present study found that simple reaction time (SRT) was slower (3.2–9.3%) in the mornings (following 24 h of sleep deprivation, and again after 8 h of recovery sleep) as compared to the evening (following 12 h of sleep deprivation). This is partly consistent with a previous reports [21, 51] showing that when straight wakefulness exceeds 16 h (typically the end of a normal day), SRT slowed down. These already slow SRTs became even slower as wakefulness was maintained throughout the night into the early morning hours leading up to 24 h of total sleep deprivation. However, the current study observed that this phenomenon did not persist when total sleep deprivation reached a maximum of 36 h, and instead, SRT showed an improvement (5.9%) compared to the 24-h time point.
Thanks for your insightful feedback on our paper. We recognize the significance of your points and we incorporated them in our revised version to improve its rigor.
-L164-168: This paragraph should clearly describe the objectives of the study: TSD (36 h), cognitive (SRT…) physical (JH) military personnel (18 male).
The text referring to non-significant interactions has been deleted in both the results and abstract sections, as you suggested.
We are deeply appreciative of the insightful comments provided on our manuscript. The reviewers' constructive feedback was instrumental, guiding us in refining and enhancing our work. After incorporating these suggestions, we believe the manuscript has become significantly stronger, more comprehensive, and better positioned to contribute meaningfully to the field.



 Neil
Neil 
 Neil
Neil