Effects of synchronisation during SiPAP-generated - sipap
There was no statistically significant association between gender nor age with total ocular, corneal and internal HOAs. Both IOP (Pearson correlation coefficient, r = 0.091, p = 0.037) and minimum keratometry (Pearson correlation coefficient, r = 0.092, p = 0.039) correlated positively with only ocular primary spherical aberration (Z04) but not with any other HOAs. Maximum and average keratometry did not correlate with any HOA (Table 2).
All subjects underwent a standardized set of investigations and a complete ophthalmic examination, including subjective refraction, letter contrast sensitivity tests and a dilated fundal examination. Visual function tests which measured monocular best spectacle corrected visual acuity (BSCVA) and contrast sensitivity (CS) were performed by trained optometrists under varying lighting conditions. High contrast BSCVA was first measured using a projector Snellen chart at 4 m under photopic conditions and converted to logMAR (Logarithm of the Minimum Angle of Resolution) scale for statistical evaluation. High contrast BSCVA was further measured under mesopic and simulated night vision conditions with the super vision test-night vision goggles (SVT-NVG) chart (Precision Vision, La Salle, Illinois) [42]. The SVT-NVG employs an NVG filter which was a dark green, low-luminance filter that is placed in front of the illuminated chart, reducing chart luminance (from 100 to 4 cd/m2) to simulate low luminance (i.e. wearing NVG). Low contrast BSCVA was measured using the 5% Sloan letter chart (Sloan charts; Precision Vision, LaSalle, IL) at 3 m. Letter contrast sensitivity was measured under mesopic and NVG conditions using the SVT-NVG. Biometry (axial length and keratometry) was measured using the Sonomed A-5500 A scan (Sonomed, Inc., Lake Success, NY). IOP was measured with non-contact tonometry (NT-3000; Nidek Co, Tokyo, Japan).
RMS = root mean square, or the square root of the mean of the squared coefficients; HOA = higher-order aberration; Total HOA RMS summarizes HOA from the third to sixth order; 95% CI = 95% confidence intervals of the mean values in the population.
This study reports the distribution of ocular, corneal and internal HOAs, their relationship with demographic and ocular factors, as well as their impact on visual function in a population of young Asians with high myopia.
To furnish your home is to furnish your life. Do it with more style at Sheely's. With a showroom that exceeds 80,000 square feet and a 150,000 square foot warehouse, that’s almost 6 acres of selection and inventory. Sheely’s has Ohio and Pennsylvania’s largest selection of furniture, appliances, lighting and accessories at everyday low prices. Sheely's provides delivery service to over a 150 mile radius including Cleveland, Akron, Canton, East Liverpool, Warren, Youngstown, New Castle, Pittsburgh, Cranberry Twp., Coraopolis and Chester, WV.
One-way analysis of variance (ANOVA) with appropriate Bonferonni post-hoc testing and independent t-tests were used to compare means between groups of continuous variables. Correlation analysis was performed to investigate the relationship between continuous variables (i.e. age, refractive error, IOP and keratometry) and wavefront aberrometry parameters.
Nvg asianfit goggles
Negative correlation between (A) Ocular and (B) Internal primary spherical aberration (Z04) and Spherical equivalent of refractive error.
Keywords: Myopia [C11.744.636], Corneal wavefront aberration [C11.744.345], Visual acuity [F02.463.593.932.901], Contrast sensitivity [F02.463.593.932.901.500]
We examined inter-racial difference in HOAs, but restricted comparison to between the 423 eyes of Chinese subjects (213 subjects) and 68 eyes of Malay subjects (34 subjects), due to the small remaining numbers of subjects of other ethnicities. On average, Malay subjects had consistently lower levels across ocular, corneal and internal HOAs compared to Chinese subjects (Table 3). The mean difference (SD) in internal total HOA RMS between the two ethnicities was statistically significant [0.0246 (0.007) μm, p < 0.001], while differences in ocular and corneal total HOA RMS did not reach statistical significance. The inter-racial mean differences (SD) in internal third order RMS [0.021 (0.006) μm, p = 0.001], fourth order RMS [0.0123 (0.004) μm, p = 0.004] and primary coma (Z±13) RMS [0.0169 (0.004) μm, p = 0.001] were also statistically significant.
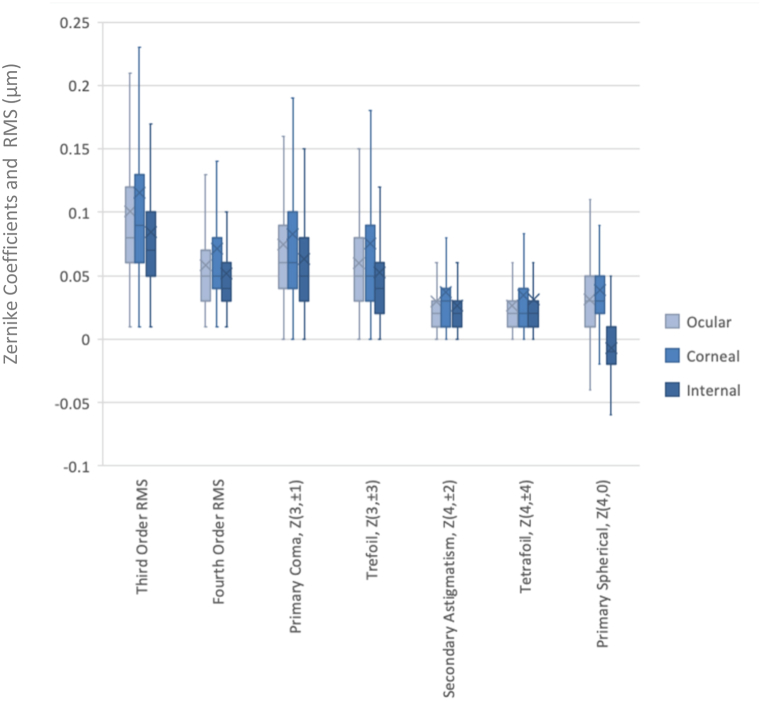
Box-and-whisker plots depicting the HOA RMS values and the distribution of Zernike Coefficients in the study population. The “X” on each bar represents the mean RMS value of the Zernike coefficient. The primary spherical (Z04) coefficient is given as a signed value.
To the best knowledge of the authors, this is one of the first studies of its kind which examines HOAs in a sizeable population of young Asian males with high myopia, demonstrating a significant correlation between HOAs and ethnicity, as well as refractive error. HOAs were associated with reduced contrast sensitivity and visual acuity when tested under low luminance settings.
Statistical analysis was performed using the Statistical Package for the Social Sciences, version 23.0 (SPSS Inc, Chicago, IL), and statistical significance was assumed at the p < 0.05 level. As HOAs are fitted across the unit circle, they vary for different pupil sizes [22,44]. To allow for meaningful inter-subject comparisons, wavefront aberrometry was calculated based on a circular pupil of 4-mm diameter, centred on each subject’s undilated pupil. Given the low correlation in ocular HOA RMS between eyes (Pearson correlation coefficient, r = 0.063), data from both eyes were used for analysis.
This study was funded by Ministry of Defence (MINDEF), Singapore. The funding organization had no role in the design or conduct of this research. The authors do not receive any funding support.
Official websites use .gov A .gov website belongs to an official government organization in the United States.
The mean (SD) age of subjects was 18.5 (1.6) years (range, 16–29) and 97.7% of the subjects (257 subjects) were male. The racial distribution of the 522 eyes of 263 subjects analysed were as follows (with percentages cited based on the number of eyes): Chinese 81.0% (423 eyes of 213 subjects); Malay 13.0% (68 eyes of 34 subjects); Indian 4.0% (21 eyes of 11 subjects); and others (e.g. Caucasian) 1.9% (10 eyes of 5 subjects). 62 eyes (11.9%) had high myopia, with SER between −6.00 D to −10.00 D; and 460 eyes (88.1%) had severe myopia, with SER ≤ −10.00 D. Mean (SD) SER was −11.85 (2.03) D (range, −6.00 to −22.38 D) and mean (SD) axial length was 28.23 (1.23) mm (range, 25.00–31.84 mm). The mean (SD) IOP was 17.1 (2.89) mmHg (range, 8.30–27 mmHg).
This study also found that higher myopia was significantly associated with a more positive ocular and internal primary spherical (Z04) aberration, but not the corneal term. Few studies have examined the association between corneal and internal aberrations with refractive error. Philip et al. reported that myopic eyes had significantly less positive total ocular primary spherical aberration and more negative internal spherical aberration, compared to emmetropic and hyperopic eyes [32]. Marcos et al. observed that in a population of young adults, higher myopia was associated with a significant increase in the corneal spherical aberration in the positive direction, while the internal spherical aberration became more negative [51]. Llorente et al. found that total ocular aberrations and corneal spherical aberration were significantly greater in young hyperopic eyes than in young myopic eyes, but internal spherical aberration did not differ significantly between the two groups [52]. Results from our study are the most consistent with findings reported by Kasahara et al. who reported that both ocular and internal primary spherical (Z04) aberration, when measured across a 6-mm pupil, were significantly higher (i.e. more positive) in highly myopic patients than those in emmetropic controls. In addition, the authors found a significant negative correlation between SER and ocular primary spherical (Z04) aberration (r2 = 0.175, p < 0.01) as well as SER and internal primary spherical (Z04) aberration (r2 = 0.274, p < 0.01) [28]. These findings may suggest that, in a high myope population, ocular primary spherical (Z04) aberrations arise primarily from internal aberrations, rather than from the cornea, which increase with worsening myopia and astigmatism. This is in contrast to the other HOAs (e.g. trefoil, coma, tetrafoil, secondary astigmatism) which arise from corneal aberrations and are instead compensated by internal aberrations [[47], [48], [49]]. The underlying reason for the relationship between internal primary spherical (Z04) aberrations and myopia is unclear, although it has been suggested that the increased internal spherical aberration in highly myopic eyes may be caused by changes in the crystalline lens, such as the steepening of anterior lens surface – similar to the age-related increase in internal spherical aberration which has been postulated by authors in previous studies [28,53].
For each micrometer increase in the magnitude of HOA, there was a deterioration of mean NVG BSCVA by 0.24 (p < 0.001) and low contrast BSCVA by 0.22 (p = 0.001) LogMAR. Similarly, for each micrometer increase in the magnitude of HOA, there was a deterioration of mean mesopic CS by 0.128 (p = 0.048) and NVG CS by 0.173 (p = 0.008) LogCS (Table 5).
To examine the associations between higher order aberrations (HOAs), visual performance, demographics, and ocular characteristics in a young Asian population with high myopia.
To account for possible collinearity between SER, ocular, corneal and internal HOAs, six linear regression models were employed, one for each visual function test: photopic BSCVA, mesopic BSCVA, NVG BSCVA, low contrast BSCVA, mesopic CS and NVG CS. Multivariate linear regression analysis demonstrated significant association between SER and all six measurements of visual function (all p < 0.001) while ocular total HOA RMS was only significantly associated with NVG BSCVA, low contrast VA, mesopic CS and NVG CS (all p < 0.05). There was however no significant association between corneal and internal total HOA RMS with any of the visual functions (Table 5).
The mean (SD) ocular, corneal and internal HOA RMS values in this study, 0.120 (0.07), 0.140 (0.12) and 0.103 (0.10) μm, respectively, were found to be slightly greater compared to that reported in a similar study by Hao et al. [50], performed also in a young, Chinese population of 40 subjects, which found corresponding mean HOA RMS values of 0.104, 0.128 and 0.098 μm. Hao et al. similarly measured HOAs on undilated 4-mm pupils using a Hartmann-Shack wavefront aberrometer. The differences in mean HOA values between the two studies, while small and likely not clinically significant, could be due to differences in refractive error in study populations.
This was a retrospective study conducted at the Singapore Armed Forces (SAF) Vision Performance Centre from March 2014 to September 2018. This study followed the tenets of the Declaration of Helsinki and was approved by the DSO-SAF Institutional Review Board, Singapore. The study population included consecutive military servicemen with high myopia detected at their pre-enlistment medical screening. Subjects with severe high myopia (defined as spherical equivalent of refractive error (SER) ≤ −10.00 D) in at least one eye and at least high myopia (SER ≤ −6.00 D) in the fellow eye were included in the study. Subjects with a history of refractive or ocular surgery, corneal reshaping treatment, ocular trauma, anterior segment disease and retinal pathology were excluded from this study.
Nvg asianfit
Unlike most previous studies which have tested only VA or CS [11,37,40,58], this study attempts to apply a wider range of visual performance tools – including the SVT-NVG and low-contrast VA – in exploring associations between HOAs and visual function. Multivariate linear regression analysis demonstrated that SER was significantly associated with all six measurements of visual function (all p < 0.001) while ocular total HOA RMS was only significantly associated with NVG BSCVA, low contrast BSCVA, mesopic CS and NVG CS (all p < 0.05) but was not significantly associated with photopic and mesopic BSCVA (Table 5). This suggests that HOAs have a greater influence on visual performance tested under low luminance and low-contrast settings. This observation corroborates with findings from other studies which noted that increased HOAs resulted in reduced contrast sensitivity function but did not affect high-contrast BCVA tested under photopic conditions [11,36,39,59,60]. These findings highlight the greater sensitivity of NVG BSCVA, low-contrast BSCVA, mesopic CS and NVG CS, compared to visual acuity testing under photopic and mesopic conditions, to determine the effect of HOAs on visual function [61].
The worldwide prevalence of myopia has increased significantly in recent years [1]. It is estimated that by 2050, 4.76 billion of the world’s population will have myopia, with 940 million people having high myopia of −5.00D or less [2]. Singapore has one of the highest rates of myopia worldwide, with incidence rates of 38.7%, 26.2% and 28% among Singaporean Chinese, Malays and Indians respectively [[3], [4], [5]], and higher rates amongst teenagers aged 14–19 years old [6]. The etiology of myopia is multifactorial, with both genetic and environmental factors contributing to its development and progression [7]. Environmental factors include close work [8], poor retinal image [7] and imagery in the peripheral retina [9]. Lower order aberrations such as myopia and regular astigmatism are easily correctable by spectacles or contact lenses [10]. However, higher order aberrations (HOAs) cannot be corrected by conventional means and have been reported to result in optical degradation [11] by reducing retinal image quality, which itself may play a role in the development of myopia [12,13].
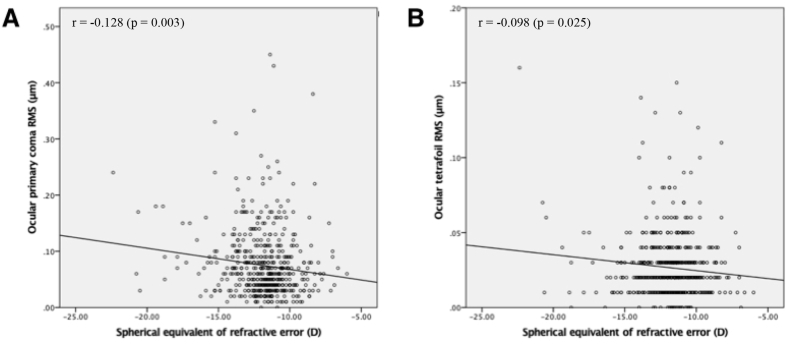
Using a similar wavefront aberrometer as in our study, Kasahara et al. examined the higher order aberrations in a population of middle-aged, Asian, high myopes (SER ≤ −8.00 D) [28] and found that the ocular total HOAs and the internal total HOAs measured across a 4-mm pupil also had negative correlation with dioptric power (r2 = 0.0864 and 0.0716, respectively). However, there was no correlation between dioptric power and individual HOA terms. Our results are also consistent with that reported by Paquin et al., who found that ocular coma occurred more frequently as one of the major aberrations among subjects with high myopia (SER from −6.00 D to −9.25D) compared to those with medium and low myopia (SER between −1.00 and −6.00D). The authors suggested that the increased coma in myopic eyes was due to a misalignment of ocular components, resulting from morphological changes in curvature, length or refractive index of ocular components with increasing myopia [34]. Our study demonstrates further that the negative correlation between spherical equivalent and ocular higher order aberrations (specifically primary coma (Z±13) and tetrafoil (Z±44) RMS) persist even in a high myope population with a narrow SER range.
Several authors have explored the relationship between HOAs and age [[14], [15], [16], [17], [18], [19], [20]], intra-ocular pressure (IOP) [21] and ethnicity [[22], [23], [24], [25]]. Total HOAs have been reported to increase with age [14,16,17,19,20] and IOP [21]. Many studies have also concluded that HOAs are highest in East Asians and lowest among Caucasians [[22], [23], [24], [25]]. However, studies which have examined the association between refractive error and HOAs have not yielded consistent results [18,22,23,[26], [27], [28], [29], [30], [31], [32]]. In particular, there is a paucity of studies examining HOA profiles among highly myopic eyes [22,28,33,34]. While it is well established that HOAs influence retinal image quality and visual performance [35], most studies have evaluated visual acuity and contrast sensitivity under mainly photopic conditions [11,[36], [37], [38], [39], [40]]. Our study team sought to better understand the determinations of HOAs and their impact on visual performance in our population of highly myopic military servicemen so as to improve training safety and vocation matching. As such, this study aimed to examine the relationship between various demographic and ocular factors with HOAs, in a population of Asians with high myopia of SER ≤ −6.00D. The relationship between HOAs and visual performance is also explored through the examination of visual acuity and contrast sensitivity, under both light and dark conditions [41].
Analysis of the RMS of individual Zernike terms with visual function revealed a significant association between the ocular third-order aberrations [namely primary coma (Z±13) and trefoil (Z±33)] and NVG BSCVA, low-contrast BSCVA as well as CS, where subjects with greater third order aberrations demonstrated poorer visual acuity and CS function (Table 6). Oshika et al. found a similar correlation between “comalike aberration” (calculated as the RMS of third order HOAs) and letter contrast sensitivity as well as low-contrast VA (tested with a 10% contrast chart) [36]. A recent study by Zhao et al. reported a similar negative correlation between CS and third order aberrations when tested using sine wave gratings at low spatial frequencies (1.5, 3 and 6 c/d) [40]. Analysis of individual Zernike terms in this study revealed a negative correlation between CS and horizontal coma (Z13) but a positive correlation between CS and vertical trefoil (Z-33) and vertical secondary coma (Z-15). The mixed (positive and negative) correlation between CS and individual Zernike terms led the authors to conclude that certain individual Zernike terms may improve visual function while others deteriorated it. Our study did not find a similar mixed trend as our data measured similarly paired modes after combining them into polar modes – e.g. combining modes primary vertical coma (Z-13) and primary horizontal coma (Z13) to primary coma (Z±13). This method of combining similarly paired modes has been demonstrated to more accurately determine the visual significance of HOAs [62]. It has also been shown that aberrations, especially in different combinations, affect visual performance in different ways [63]. Our findings show that both the combined vertical and horizontal coma (Z±13) as well as combined vertical and oblique trefoil (Z±33) RMS reduced low-contrast BSCVA, but only the latter influenced NVG BSCVA and CS. Of the third-order HOAs, increasing trefoil (Z±33) RMS reduced low contrast BSCVA to a greater extent as compared to primary coma (Z±13) RMS (Beta = 0.134 and 0.124, respectively) (Table 6). Fernandez-Sanchez et al. studied the impact of third-order HOAs in healthy eyes by inducing aberrations of coma and trefoil with purpose-designed soft contact lenses of different degrees [64]. The authors found that with the highest level of induced coma (1.03 μm) and trefoil (0.96 μm) high-contrast, low-contrast visual acuity as well as contrast sensitivity was significantly reduced. This effect was greater in eyes with induced trefoil compared to coma across all three parameters, although the difference did not reach statistical significance. This is consistent with our study results, which further demonstrate that inherent primary coma and trefoil in high myopes, albeit of lower magnitudes, may lead to poorer low contrast visual acuity.
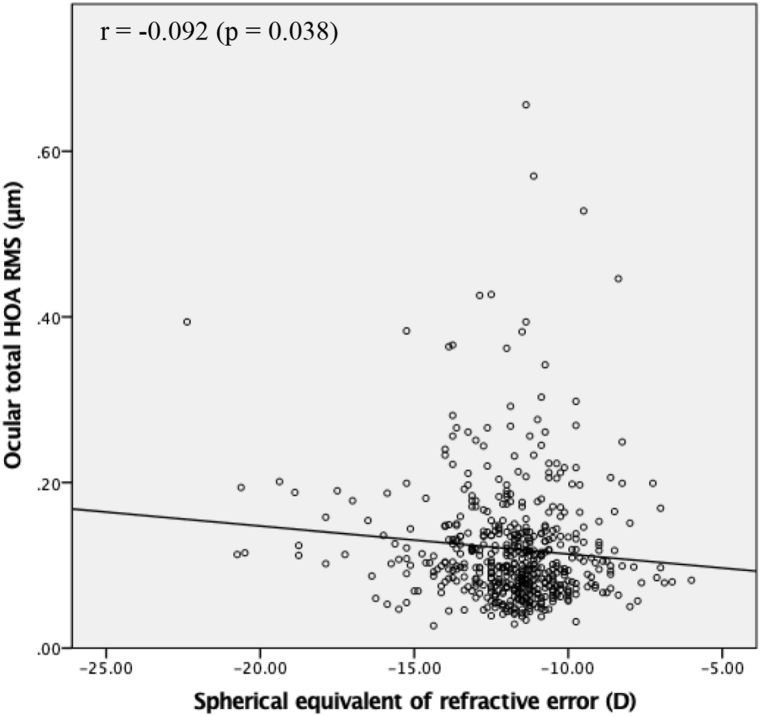
SER correlated significantly with ocular total HOA (Pearson correlation coefficient, r = −0.092, p = 0.038), but not corneal or internal total HOA (Fig. 2, Table 4). Analysis of the individual Zernike coefficients revealed significant negative correlation between SER and ocular primary coma (Z±13) RMS (r = −0.128, p = 0.003), tetrafoil (Z±44) RMS (r = −0.098, p = 0.025) and primary spherical aberration (Z04) (r = −0.130, p = 0.003) (Fig. 3, Fig. 4A, respectively and Table 4). Of the corneal and internal terms, SER was negatively correlated with only internal primary spherical aberration (Z04) (r = −0.166, p < 0.01) (Fig. 4B, Table 4). There was no significant difference in HOA values between eyes with high myopia (SER -6.00 D to > −10.00 D) and severe high myopia (SER ≥ −10.00 D).
Both ocular and corneal primary spherical aberration (Z04) were predominantly positive with mean (SD) values of 0.032 (0.03) μm and 0.038 (0.03) μm, respectively. In contrast, 50.8% of eyes had a negative primary spherical aberration (Z04) term, with a mean (SD) value of −0.007 (0.05) μm.
Our study showed that Malay eyes had consistently lower levels of HOAs compared to Chinese eyes, with the mean differences in internal total HOA RMS, third order RMS, fourth order RMS and primary coma (Z±13) RMS reaching statistical significance. Importantly, there was no significant difference in the mean SER of both groups: mean (SD) SER of Chinese eyes −11.83 (1.99) D versus Malay eyes −12.16 (2.19) D (p = 0.25). Ethnic variations in HOAs have been previously documented, with studies observing that HOAs were highest among East Asian eyes and lowest in Caucasians [[22], [23], [24], [25]]. When measured across a 6-mm pupil diameter with a Hartmann-Shack wavefront aberrometer, mean total HOA RMS among healthy Asian subjects have been reported to range from 0.35 to 0.55 μm [21,22,24,25,54,55] as compared to mean values between 0.305 and 0.327 μm among non-Asians [23,44,56,57]. This may be due to inherent racial differences in the curvature or shape of the cornea, or in internal ocular components. Lim et al. postulated that the lack of corneal prolateness in Eastern Asians compared to that reported in white populations may translate into greater positive spherical aberration [24]. In a study of 273 school-going children with a mean age of 9 years, also conducted in Singapore, Carkeet et al. found that Malay subjects had significantly lower total HOA RMS, primary coma RMS and spherical aberration compared to Chinese subjects [22]. Our study’s results suggest that such racial differences in HOAs among children were similarly found in young adults with high myopia.
Primary coma (Z±13) RMS had the greatest mean value across ocular, corneal and internal measurements. Ocular, corneal and internal third order terms (primary coma and trefoil RMS) had significantly higher mean values compared to 4th order terms (secondary astigmatism RMS, tetrafoil RMS, primary spherical aberration) (all p < 0.001) (Fig. 1).
In our population of highly myopic eyes, we found that increasing myopia was associated with greater ocular total HOA, with effects extending to primary coma (Z±13) and tetrafoil (Z±44) RMS (Fig. 3). Studies do not agree on the effect of refractive error on HOAs, with some reporting greater HOAs amongst both myopes [18,[27], [28], [29], [30]] and hyperopes [23,32], while some found no differences among different refractive groups [22,31]. It is challenging to postulate clear reasons for these conflicting conclusions, due to the incongruity in the methodologies (e.g. differences in devices used to measure HOAs, pupil sizes across which HOAs were measured, statistical comparison, etc.) and the study populations (e.g. varying distribution of age, race, refractive error, etc.) of these studies.
There are limitations in this study. Firstly, our study comprised mainly young, male participants of Chinese ethnicity with high myopia. Given the narrow demographic and SER range of our subjects, our findings may not be generalisable to other populations and wider ranges of SER. Secondly, our study only examined HOAs measured across undilated 4-mm pupils. It is acknowledged that pupillary diameter influences the association between refractive error and visual performance [[65], [66], [67], [68]], as well as the magnitude of HOAs, with significantly greater HOAs when measured across larger pupil sizes (e.g. 6-mm pupil sizes) [34,65]. Hence, this may limit the comparison of HOA values across studies when there are differences in pupil sizes across which aberrations are measured. Finally, this study’s design may only determine associations and correlations between the various ocular factors and HOAs. Further studies are needed to determine causality relationships.
The total HOA summarizes higher order aberration from the third to sixth order. The mean (SD) RMS values for ocular, corneal and internal total HOAs were 0.120 (0.07) μm (95% CI, 0.113 to 0.126), 0.140 (0.12) μm (95% CI, 0.130 to 0.151) and 0.103 (0.10) μm (95% CI, 0.095 to 0.112), respectively (Table 1).
303 consecutive pre-enlistees with SER ≤ −10.00 D in at least one eye were initially recruited for this study. 37 subjects with incomplete or unavailable examination data and a further 3 subjects who were on orthokeratology lenses were excluded. Of the remaining 263 subjects, 4 eyes with SER ≥ −6.00 D on subjective refraction were further excluded. A total of 522 normal eyes of 263 subjects were included in final analysis.
Wavefront aberrometry measurements were performed with the eye undilated, using a Hartmann–Shack wavefront aberrometer (KR-1W, Topcon Co., Tokyo, Japan) under fixed, mesopic lighting conditions (measured illuminance of 1.6 Lux, using the Sekonic Spectromaster C-7000 Spectrometer, SKU: 401-710). Participants were presented with a fixation target image of a red house, with brightness pre-set at “Level 4”, the brightest of 4 levels. Ocular accommodation was controlled for by presenting a blurred target image prior to it coming into focus. The following wavefront aberrometry parameters were recorded: ocular, corneal and internal total HOA root-mean-square (RMS) (computed for third to sixth Zernike terms), third order RMS, (fourth order RMS, primary coma RMS (computed for the Zernike terms Z±13), trefoil RMS (computed for the Zernike terms Z±33), secondary astigmatism RMS (computed for the Zernike terms Z±24), and tetrafoil RMS (computed for the Zernike terms Z±44). The corresponding Zernike coefficient for primary spherical aberration (Z04) was also reported with its sign. The accuracy of this device in measuring aberrations has been previously established [43].
When individual ocular RMS and Zernike coefficients were substituted into the model in place of ocular total HOA RMS, trefoil (Z±33) RMS was significantly associated with NVG BSCVA (beta = 0.119; p = 0.040), low contrast BSCVA (beta = 0.134; p = 0.020) and mesopic CS (beta = −0.126; p = 0.028). Primary coma (Z±13) RMS was significantly associated with low contrast BSCVA (beta = 0.124; p = 0.032) (Table 6).
Multiple linear regression analyses were performed to assess the relationship between visual function (dependent variables) and SER, as well as with wavefront aberrometry parameters (independent variables).
Greater HOAs were associated with Chinese ethnicity and more negative SER in a young Asian population with high myopia. Greater HOAs were associated with poorer visual performance in low luminance and reduced contrast conditions.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
522 eyes of 263 consecutive subjects with severe high myopia (defined as spherical equivalent refraction [SER] ≤ −10.00D) in at least one eye, and high myopia (SER ≤ −6.00D) in the fellow eye, [mean (SD) SER −11.85 (2.03D)] were analysed. The mean (SD) age of subjects was 18.5 (1.6) years. Chinese eyes had significantly greater internal total HOA root-mean-square (RMS) compared to Malay eyes [mean difference (SD) 0.0246 (0.007) μm, p < 0.001). More negative SER was associated with greater ocular total HOA (p = 0.038), primary coma (p = 0.003) and tetrafoil (p = 0.025) RMS, as well as more positive ocular (p = 0.003) and internal primary spherical aberration (p = 0.009). Greater ocular total HOAs was associated with reduced visual acuity in simulated night conditions and low contrast, decreased contrast sensitivity under mesopic and simulated night conditions (all p < 0.05).
Comparison of HOA values across studies remains challenging due to the use of different devices for determining aberrations and Zernike indices. Studies also differ in various aspects, including the pupil size across which the wavefront aberrations are measured, subject demographics, as well as the visual and refractive status of subjects. Measuring HOAs across a 4-mm pupil using a Hartmann-Shack wavefront aberrometer, our study found that HOAs decreased in magnitude as the order of aberration increased, similar to that previously described in literature [[23], [24], [25],[44], [45], [46]]. The consistently lower ocular Zernike terms compared to corresponding corneal measurements may demonstrate partial compensation of corneal HOAs by the internal optics of the eye, from structures such as the posterior cornea and the crystalline lens. This is also in agreement with prior literature which suggests that there is a degree of compensation between corneal and internal aberrations for young eyes, as evidenced by corneal aberrations being higher than the total ocular aberrations [[47], [48], [49]].
This was a retrospective review of military pre-enlistees conducted between March 2014 to September 2018. Visual acuity and contrast sensitivity were tested under photopic, mesopic and simulated night conditions. Ocular, corneal and internal HOAs were measured with a Hartmann–Shack wavefront aberrometer (KR-1W, Topcon Co., Tokyo, Japan).



 Neil
Neil 
 Neil
Neil