HatchMed Email Format - hatchmed
EEA sizermeaning
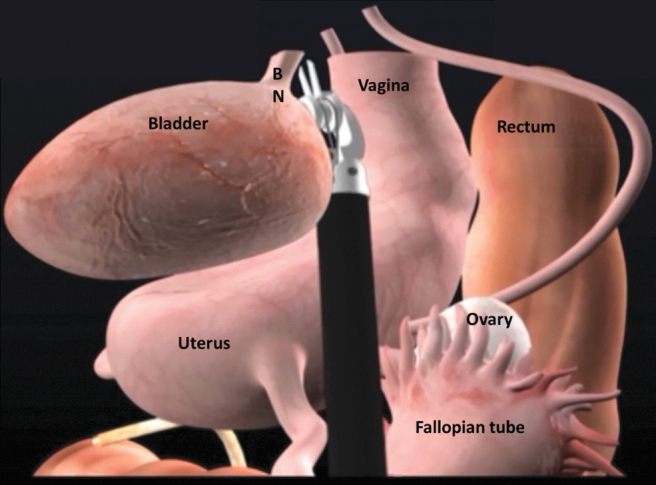
Schematic illustration of posterior bladder dissection in POSRC. BN = bladder neck; POSRC = pelvic organ-sparing radical cystectomy.
The da Vinci Xi (Intuitive Surgical) robotic system is docked with the surgical assistant operating from the patient's left side. We utilize fenestrated bipolar in the left robotic arm, monopolar scissors in the right arm, and a Vessel Sealer in the fourth robotic arm.
Using the fourth arm to retract the bladder anteriorly, the bladder pedicles are placed on stretch and away from the external iliac vessels. The superior vascular pedicles to the bladder are divided using the Vessel Sealer or locking clips (Supplementary Video S3). Branches from the inferior pedicles are then identified, separated into small packets, sealed or clipped, and divided. Connective tissues and small perforating arteries can be dissected and controlled with electrocautery.
All patients follow a standardized enhanced recovery after cystectomy pathway postoperatively. Components of this pathway include removal of nasogastric/orogastric tube at the end of the procedure before the patient leaves the operating room, discontinuation of antibiotics within 24 hours, early enteral feeding, aggressive mobilization and incentive spirometry, active prevention of nausea, narcotic-sparing multimodal pain management, and prophylaxis of thromboembolic events. Patients are started on sips of water and ice chips on the day of surgery. They are subsequently advanced to full liquid diet on postoperative day (POD) 1 and regular diet on POD 2 or 3 if patient tolerates full liquid without abdominal distention or nausea. Selective opioid receptor blockade with alvimopan is initiated preoperatively and continued until return of bowel function for up to 14 doses postoperatively. Patients are mobilized out of bed on POD 0. Ambulation with assistance begins on POD1. Narcotic-sparing pain management regimen composes of TAP block preoperatively, scheduled acetaminophen, nonsteroidal anti-inflammatory medication, and gabapentin. Oral and intravenous opioid medication may be given as needed for breakthrough pain. Gastrointestinal prophylaxis with a proton pump inhibitor and deep venous thrombosis (DVT) prophylaxis with low molecular weight heparin are instituted immediately postoperatively. Pharmacologic DVT prophylaxis is continued for 28 days in the postoperative period.
Neobladder-vaginal fistula has been reported in women undergoing classical radical cystectomy at a rate of 3%–5%.28,34–36 Although neobladder-vaginal fistula is uncommon in POSRC, there are additional steps that can prevent the risk of fistula. First, care must be taken to avoid overlapping suture lines between the vagina and bladder neck. Second, a pedicled omental flap can be harvested to reinforce the vaginal closure and act as an interposing layer between the vaginal stump and urethro-ileal anastomosis, especially in the case of prior pelvic radiation (Supplementary Video S6). An omental flap is easy to harvest and has a reliable blood supply. The greater omentum is dissected from the transverse coon and greater curvature of the stomach to form an omental flap based on the left or right gastroepiploic artery, whereas retaining the gastroepiploic arch. The flap is then tunneled to the pelvic floor and secured to the endopelvic fascia with absorbable barbed suture (Fig. 10).
The author(s) have received and archived patient consent for video recording/publication in advance of video recording of procedure.
Truck Dockboard, 6000 Lb. Capacity, 72 Inch x 30 Inch Size, Aluminium | AG7MWZ | Delivery to the UK & Channel Islands | sales@raptorsupplies.co.uk | 0203 ...
Sea Salt & Vinegar Flavour Popped Potato Snacks. Trade Pricing Available. £17.508 x 85g. £2.57/100g. £21.00 incl VAT. In Stock. Add. Save to List. Favourite.
In this case, it is usually inserted into the superior vena cava, or ... Liberty Cycler. Innovative device with PIN technology (automatic inline ...
Some posterior dissection of the vagina may need to be performed to bring the posterior vaginal wall toward the anterior remnant for vaginal closure (Supplementary Video S5). The vaginal reconstruction can be performed in a clamshell manner with two layers of running absorbable sutures as shown in Figure 9. Rolling the vaginal remnant into a tube in an effort to preserve vaginal length without adequate preservation of the anterolateral walls can lead to a narrow vaginal canal that is not suitable for sexual intercourse and higher risk of breakdown. At the completion of vaginal reconstruction, manual examination should be done to ensure the vaginal defect is completely closed and intact.
The uterus, the cardinal ligaments containing the uterine arteries, and supporting ligaments are spared (Fig. 7). The previously transected distal ureter is dissected free and delivered under the uterine artery to preserve the cardinal ligament. Limited dissection of the uterus is performed posteriorly, leaving the uterosacral ligaments undisturbed.
A 30° lens is used during the procedure. Once ports are placed, the surgeon should orient to the female pelvic anatomy. Dissection usually proceeds with identification and mobilization of the left ureteral (Supplementary Video S1). We incise the white line of Toldt and develop the relatively avascular plan to separate the left colon from the pelvic side wall and reflect the sigmoid colon medially and superiorly out of the surgical field. The left ureter is identified as it crosses the left common iliac artery. The peritoneum overlying the ureter is incised. The ureter is freed from its surrounding structures while preserving adequate periureteral tissue to maintain the vascular supply to the ureter. As the ureter is dissected distally, the adnexa are lifted cephalad, along with the infundibulopelvic (IP) suspensory ligament. The ureter is mobilized distally to the level of the uterine artery, which courses medially and over the ureter. The pelvic vasculature is shown in Figure 2. The ureter is then doubly ligated with locking clips and transected without thermal energy. A suture may be pretied to the crotch of the proximal clip to facilitate its identification and mobilization during the urinary diversion portion. The ureter is dissected free of its cephalad attachments enough to reach the urinary diversion reconstruction. Excess dissection of the ureter should be avoided to minimize devascularization of the ureter. The right ureter is mobilized and divided using a similar technique.
A total of six ports are used during the procedure as shown in Figure 1. The 8-mm camera port is positioned ∼5 cm cephalad to the umbilicus. After the camera port placement, a 30° robotic camera is inserted. The abdomen is inspected for injury or adhesion. Subsequent ports are placed under direct observation. Three 8-mm robotic ports are placed in a horizontal line 1 fingerbreadth caudal to the camera port. The left and right ports are approximately one handbreadth from the midline. The right lateral port for the fourth robotic arm is placed at the level of the anterior axillary line. A 12-mm AirSeal® assistant port (ConMed) is placed in the left upper quadrant and another 12-mm assistant port is placed in the left anterior axillary line at the level of the umbilicus. The patient is then placed in 28° steep Trendelenburg position.
Pedicled omental flap is brought down to the pelvis to reinforce the vaginal closure and interposes between the vagina and urethro-ileal anastomosis in case of ONB.
Franco Gaboardi, Marco Grillo, Giuseppe Saitta, Giovanni Passaretti, Salvatore Smelzo, Nazareno Suardi, and Giovannalberto Pini.
In patients with prior hysterectomy or those who require classical radical cystectomy, the removal of reproductive organs and their supporting tissues may result in weakening of the pelvic floor and may put patients at risk of bowel herniation through the vaginal wall. In addition, patients who undergo ONB after classical radical cystectomy may be at high risk of urinary retention, potentially from angulation of the neobladder-urethral anastomosis caused by backward displacement of the neobladder. One way to reduce the risk of pelvic organ prolapse and urinary retention in patients who undergo ONB is to perform concomitant abdominal sacropolpopexy after RARC and pelvic lymph node dissection are completed (Supplementary Video S7). The sigmoid colon is retracted atraumatically to the left side to expose the sacral promontory. An incision is made in the posterior peritoneum over the sacral promontory to expose the anterior spinous ligament, extending caudally along the right lateral aspect of the rectum to the posterior vagina to create a longitudinal peritoneal flap. Using an EEA sizer as vaginal probe to identify the apex of the vagina, the anterior leaflet of a Y-shaped soft polypropylene mesh is sutured to the anterior vaginal remnant using a running 2–0 barbed suture. The posterior leaflet of the mesh is sutured to the posterior vaginal remnant in a similar manner. The tail of mesh is then secured to the anterior spinous ligament at the level of the sacral promontory using interrupted nonabsorbable sutures such as 2–0 Gore-tex suture. Care must be taken to avoid suturing the middle sacral vessel traversing over the promontory and excessive tension of the mesh. The previously created peritoneal flap is then used to cover the mesh using running 2–0 Vicryl sutures (Fig. 11).
EEA sizerhysterectomy
Upgrade your shop with the reliable performance of Bosch Filters. Take advantage of our competitive pricing and unlock the benefits of our exclusive eXtra ...
Official websites use .gov A .gov website belongs to an official government organization in the United States.
This section collects any data citations, data availability statements, or supplementary materials included in this article.
17 Jun 2018 — This document describes how to unlock a volume group with an error like: 0516-1201 lsvg: Warning: Volume group is locked.
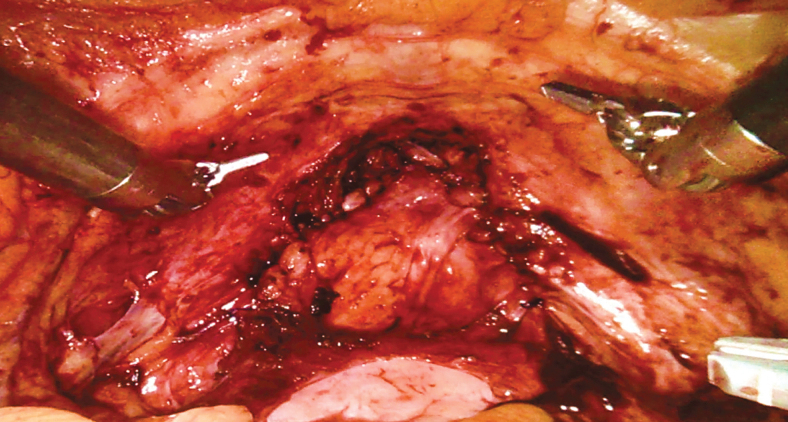
After the ureters are mobilized, the uterus is retroverted, the peritoneum over the vesicouterine pouch is incised transversely. With the bladder lifted anteriorly, the avascular plan between the anterior surface of the uterus/vagina and the posterior surface of the bladder is developed (Fig. 5). The dissection continues caudally to the level of the bladder neck as illustrated in Figure 6. Care should be taken with dissection around the cervix because there are dense connective tissues at this point. Thinning of the anterior vaginal wall or the bladder should be avoided. With the anterior vagina separated from the posterior bladder, the lateral perivaginal space is developed bilaterally.
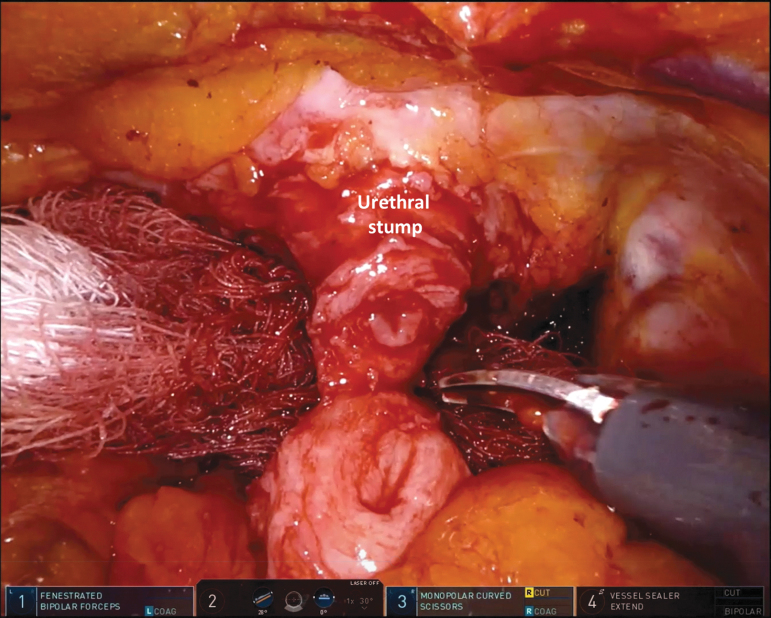
The distal dissection of the bladder neck and proximal urethra is carefully performed to preserve the anterior vagina and periurethral support (Supplementary Video S4, Part 2). The endopelvic fascia is identified, preserved, and serves as a reference for the pelvic floor. Dissection continues anterior to this plane in a caudal direction. Once the bladder neck is separated from the anterior vagina distally, the bladder is mobilized anteriorly as described in the previous section. The location of the bladder neck can be identified using the balloon of the urethral catheter for reference. Connective tissue attachment can be separated using sharp dissection and electrocautery. The DVC is divided sharply anteriorly. Care is taken to preserve the endopelvic fascia and supporting periurethral attachment to the distal third of the urethra to optimize continence with ONB reconstruction (Fig. 8). Once the urethra is transected sharply, the urethral catheter is clamped with a locking clip and divided to minimize risk of tumor spillage. Circumferential full-thickness proximal urethral margin is sent for intraoperative frozen section to rule out malignancy at the urethra margin. Since the vagina is not opened, the specimen is placed in an endocatch bag. The opening of the bag is closed with double locking clips to prevent any tumor spillage and placed in the abdomen. Our techniques of robotic pelvic lymphadenectomy and intracorporeal urinary diversion have been described previously.31–33
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
The preoperative work-up for a patient with bladder tumor starts with a detailed history and physical examination followed by urine cytology, examination under anesthesia, and TURBT as described in previous section. Screening for smoking and initiation of treatment for smoking cessation should be done at the initial evaluation. Laboratory studies, such as complete blood count, chemistry profile, alkaline phosphatase, and a coagulation panel must be performed. Assessment of the upper tract can be done with CT or MRI urography or retrograde ureteropyelography at the time of transurethral resection. Complete staging evaluation includes imaging of the chest, abdomen, and pelvis with either CT or MRI. Bone and brain imaging are only done if patient has clinical symptoms or laboratory indicators, such as abnormal alkaline phosphatase, concerning for bone or brain metastases. Patient should be counseled regarding different types of urinary diversion, possible complications, risks, benefits, and anticipated lifestyle and psychologic changes. Patient should meet with an enterostomal therapist and have stoma site marking preoperatively even when ONB is planned.
Right pelvic vasculature in relation to right distal ureter. The ureter is seen coursing over the right common iliac artery and anterior to the hypogastric artery (also known as internal iliac artery).
Home > R&D Batteries Inc. In Stock. There are no items for this manufacturer. Z7_61MAH0820101F0Q301IHRM10D2. Web Content Viewer. Component Action Menu.
After general anesthesia induction, a nasogastric or orogastric tube is placed to decompress the stomach intraoperatively and removed at the completion of the procedure. The patient is placed in supine split-leg position with the arms tucked to the side. Care must be taken to ensure all pressure points are adequately padded. The patient is secured to the operating table with nonslipping pad and chest strap. The patient will be in 28° steep Trendelenburg position during the case, which displaces the bowel cephalad and provides easy access to the pelvis. After patient is positioned and secured to the table, the table is tilted temporarily to steep Trendelenburg position to ensure that patient does not slide toward the head of the table and patient's ventilatory dynamics tolerate the extreme position. The table is then put back in neutral position for port placement.
EEAStapler
Our medical register, which lists all doctors registered with us to practise medicine in the UK. You can search the register for a doctor here.
Early postoperative rehabilitation program includes inpatient evaluation and education by wound ostomy nurses (if applicable), physical, occupational, and respiratory therapists. Postoperative follow-up and drain management are based on the type of urinary diversion patients undergo.
Antegrade anterior vaginectomy and urethral dissection. An EEA sizer is used to identify the vaginal wall and maintain pneumoperitoneum. EEA = end anastomosis.
da Vinci Xi port configuration for radical cystectomy with surgical assistant positioned on the patient's left side. C = camera port.
Radical cystectomy is the primary treatment option for nonmetastatic muscle-invasive urothelial carcinoma of the bladder (MIBC).1–3 The current standard of care is to offer cisplatin-eligible patients cisplatin-based neoadjuvant chemotherapy (NAC) before radical cystectomy given demonstrated benefits of NAC on cancer-specific mortality and all-cause mortality rates.4–6 Other indications include non-muscle invasive bladder cancer (NMIBC) with factors associated with high risk of progression to muscle-invasive disease such as variant histology report, carcinoma in situ or lymphovascular invasion7,8 in addition to high-risk NMIBC that persists or recurs despite following two induction cycles of intravesical bacillus Calmette Guerin (BCG) or BCG maintenance.3,9–12 In the context of organ-confined bladder cancer, radical cystectomy encompasses three surgical components—extirpative surgery, bilateral lymphadenectomy, and urinary diversion. Bilateral pelvic lymphadenectomy, including removal of common, internal iliac, external iliac, and obturator nodes, is an important part of a radical cystectomy and has been shown to improve control of local and regional disease and provide better long-term oncologic outcomes.13,14 This report will focus on the techniques and outcomes of the extirpative surgery only.
If present, the female pelvic organs can be identified as demonstrated in Figure 3. A medium end anastomosis (EEA) sizer is used for uterine manipulation. Alternatively, a sponge stick can be used. The peritoneum over the vesicouterine pouch is incised. The plane between the anterior vagina and the posterior bladder is developed and continues distally to the level of the bladder neck. With the uterus anteverted and laterally displaced to the contralateral side, the IP suspensory ligament, the ovarian pedicles, and the broad ligaments are identified and divided with the Vessel Sealer. The uterine arteries are ligated with locking clips and divided. Next, peritoneum lateral to the medial umbilical ligaments is incised from the anterior abdominal wall to join the peritoneal dissection over the broad ligament. The paravesical space can be developed with blunt dissection and carried caudally to expose the endopelvic fascia. Next with the uterus anteverted, the peritoneum over the rectouterine pouch is incised and connected with the lateral dissection. This step helps to define the bladder pedicles. In the absence of any cervical pathology report, transcervical hysterectomy may be performed if desired to maximize vaginal length. With the aid of a sponge stick in the vagina, the uterine fundus is transected at the level of the posterior fornix at the level of the cervical insertion. Posterior dissection continues caudally to the level of the bladder neck.
View of the pelvis after organ-sparing cystectomy has been performed. EF = endopelvic fascia and pubourethral ligament are intact; US = urethral stump.
EEAsizers Medtronic
Alvin C. Goh, Andre Abreu, Miguel Mercado, Rene Sotelo, Golena Fernandez, Monish Aron, Inderbir Singh Gill, and Mihir Desai.
Modifications to classical radical cystectomy are described hereunder for ONB reconstruction (Supplementary Video S2, Part 2). By definition, an adequate urethral stump is required for ONB. Sparing the vagina, uterus, and their supporting structures improves voiding function by preserving support for the ONB, preventing its backward displacement and angulation of the neobladder-urethral anastomosis.28–30 In addition, preservation of the vagina and uterus help to preserve the autonomic nerves along the lateral wall of the vagina, which may help to improve voiding and sexual function outcomes.30
"Shop locally at 22211 Dewdney Trunk Rd., Maple Ridge, 604-463-2388 Order by phone or visit us here online! Buy Online, Pick-up In Store!
Retrospective studies and prospective RCT have compared oncologic outcomes and complication rates between RARC and ORC. ORC and RARC have comparable oncologic controls and complication rates; RARC is associated with lower blood loss, transfusion rate, and shorter hospital stay.16,18,41 There is a paucity of studies comparing classical radical cystectomy and POSRC cystectomy in female patients, even more limited data with robotic approach. Similarly, functional outcomes among women undergoing radical cystectomy for bladder cancer are poorly studied. In a systematic review by Smith et al., only 40% of studies assessed sexual function in women using validated questionnaires.42 Table 1 summarizes oncologic, urinary function, and sexual function outcomes from select retrospective studies of women undergoing POSRC and ONB urinary diversion.
Lysol All Purpose Cleaner Multi Surface Cleaner Lemon 800ml – Help keep a healthier home top to bottom with Lysol Multi-Surface Cleaner. This pourable cleaner can be used directly on stains for spot cleaning, or diluted in water for use on large surfaces like floors. Pour directly on stains for spot cleaning. Kills 99.99% of Viruses & Bacteria*. Provides long lasting freshness. $3.27 Each. Maple Ridge Janitorial Supplies
The patient is prepped and draped from the xiphoid process to the perineum, including the vagina, and lateral to the bilateral anterior axillary lines. An 18F urethral catheter is placed in the sterile field.
Keywords: robotic radical cystectomy, female cystectomy, bladder cancer, pelvic organ-sparing radical cystectomy, surgical techniques
Open and robot-assisted radical cystectomy (RARC) have comparable oncologic outcomes and complication rates when done at experienced centers. The largest randomized control trial (RCT) to date is the RAZOR trial, which showed that RARC is noninferior to open radical cystectomy (ORC) in terms of 3-year progression-free survival (68.4% vs 65.4%),15 overall survival (73.9% vs 68.5%),15 adverse events (67% vs 69%),16 and quality-of-life (QOL) outcomes.16 A Cochrane review of five other published RCT comparing ORC and RARC showed no difference between two surgical approaches regarding time to recurrence, positive surgical margin rates, major postoperative complications, and QOL. The study found RARC may result in lower transfusion rate and shorter hospital stay.17 For both approaches, surgeon experience and institutional volume strongly predict surgical outcomes.18 The choice of surgical approach should be based on the surgeon's experience with RARC, other previous robot-assisted surgeries, or the presence of an experienced mentor to train junior surgeons.
A functional urethral stump, periurethral supporting tissue attachment to the distal third of the urethra, and the endopelvic fascia should be preserved in patients undergoing ONB. ONB = orthotopic neobladder.
CIC = clean intermittent catheterization; DSS = disease-specific survival; FSFI = female sexual function index43,44; IQR = interquartile range; NR = not reported; OS = overall survival.
Patients follow a standardized enhanced recovery clinical care pathway involving preoperative preparation and postoperative management. Preoperative bowel preparation depends on the segment of bowel used for planned urinary diversion. Patients undergoing small bowel diversion do not receive any bowel preparation. For urinary diversion using colon, patient receive a mechanical bowel preparation with magnesium citrate. All patients are placed on a clear liquid diet and carbohydrate loading for 24 hours before surgery. Patients receive one dose of alvimopan, a μ-opioid receptor antagonist, just before surgery to accelerate gastrointestinal recovery after surgery unless there is a contraindication, such as the use of therapeutic doses of opioids for more than seven consecutive days immediately before the starting dose.1,25 A regional transversus abdominis plane (TAP) block is placed in the preoperative area. Patients receive perioperative antibiotics in accordance with the American Urological Association (AUA) Antimicrobial Prophylaxis guideline.26 Unless a drug allergy to cephalosporins is present, the authors typically administer cefotetan within 60 minutes of incision. Patients are placed on mechanical and pharmacologic prophylaxis, that is, intermittent pneumatic compression on lower extremities and subcutaneous heparin, before induction of general anesthesia to prevent thromboembolic complications.1,27
The Pasadena consensus panel on best practices in RARC suggested that there is no absolute contraindication for RARC.18 The panel recognizes that there are certain challenging cases that should be performed by surgeons with extensive experience in RARC. These cases include obese patients, those with multiple prior lower abdominal surgeries, and those with prior pelvic radiation. Prior studies have shown that obese patients have similar operative times, blood loss, and complication rates as patients with normal body mass index undergoing RARC.37,38 In general, the authors have not found the need to modify our technique in obese patients and the use of bariatric trocars is rarely necessary. On the contrary, RARC in obese patients may help to circumvent some of the challenges with surgical exposure and access to the deep pelvis encountered during ORC. Patients with prior abdominal surgeries may have significant adhesion. Hasson technique is preferred for access during initial insufflation and trocar placement. Extensive laparoscopic or robotic lysis of adhesion may be needed before complete trocar placement. In case of prior pelvic radiation, care should be taken with posterior dissection to avoid rectal injury. In addition, patients should be counseled on the increased risk of complications and urinary function after ONB caused by poor tissue qualities from prior radiation.39,40
Classical radical cystectomy in a female patient includes total anterior pelvic exenteration inclusive of the bladder, uterus, fallopian tubes, ovaries, anterior vaginal wall, and urethra.1 Since the early 2000s, adoption of orthotopic neobladder (ONB) in women and an effort to improve postoperative sexual and urinary function have motivated urologists to explore less radical surgery. This effort is supported by the fact that direct involvement of the gynecologic organs at the time of radical cystectomy only occurs in around 2.6%–7.5% of women.19–22 Pelvic organ-sparing radical cystectomy (POSRC) refers to the preservation of the uterus, fallopian tubes, ovaries, and anterior vagina, and urethra. The most important factor in choosing to preserve organs is that cancer control is not compromised. Patient selection, therefore, is paramount.
Radical cystectomy is the standard of care for patients with nonmetastatic high-risk bladder cancer. Robotic approach to radical cystectomy has been developed to reduce perioperative morbidities and enhance postoperative recovery while maintaining oncologic control. Classically, radical cystectomy in female patient entails anterior pelvic exenteration with removal of the bladder, uterus, fallopian tubes, ovaries, anterior vaginal wall, and urethra. Pelvic organ-sparing radical cystectomy has been adopted in carefully selected patients to optimize postoperative sexual and urinary function, especially in those undergoing orthotopic urinary diversion. In this article, we describe our techniques of both classical and organ-sparing robot-assisted laparoscopic radical cystectomy in female patients. We also review patient selection criteria, perioperative management, and alternative approaches to improve operative outcomes in female patients.
What areEEAsizers used for
Next, anterior dissection of the bladder is performed. The median umbilical ligament is divided as proximally as possible with electrocautery. The dissection is carried caudally over the anterior surface of the bladder to the pubic symphysis to develop the space of Retzius. The location of the bladder neck can be identified using the balloon of the Foley catheter for reference. The dorsal venous complex (DVC) anterior to the urethra is divided sharply. Hemostasis can be achieved with bipolar cautery or a DVC stitch. Complete urethrectomy can be performed intracorporeally (Fig. 4 and Supplementary Video S4, Part 1). If an orthotopic urinary diversion is planned, the urethra is transected sharply without electrocautery just distal to the bladder neck to ensure preservation of a functional urethral stump. Once the urethra is transected, the urethral catheter is clamped with a locking clip before division to minimize the risk of tumor spillage. The specimen is placed in a 15-mm specimen bag and extracted through the vaginotomy.
MD0301 - Delmarva Power |150671|. Please help us support all the locations below that MD0301 - Delmarva Power supports on Wreaths Across America day. Sponsor ...
Address correspondence to: Hong Truong, MD, MS, Department of Surgery, Memorial Sloan Kettering Cancer Center, New York, NY 10065-6007, USA truongh1@mskcc.org
MAC Clinical Research is the UK's leading clinical trials organisation. As an award winning healthcare organisation, we are dedicated to developing new and ...
Selection of appropriate candidates for POSRC relies on a thorough preoperative evaluation, including gynecologic history, menopausal status, history of cervical cancer screening, abnormal vaginal bleeding, family history of breast/ovarian cancer, sexual function, and, if applicable, fertility goal. Patients who may benefit most from POSRC are those with good baseline functional status and surgical fitness (usually those of younger age but advanced age is not a contraindication), pre- or perimenopausal, sexually active, and in whom an ONB is planned. Relative contraindication may be those at risk of hereditary ovarian, endometrial, and cervical cancer such as BRCA1/2 mutation carriers and those with Lynch syndrome. Risk-reduction surgeries such as hysterectomy and salpingo-oophorectomy after childbearing and over the age of 40 have been recommended for these patients; thus, they are not appropriate candidates for POSRC.23,24 Bimanual examination under anesthesia must be performed before and after transurethral resection of bladder tumor (TURBT) for clinical staging and evaluation of concomitant gynecologic condition such as pelvic organ prolapse. TURBT must take note of tumor location, specifically evaluating for tumor involvement of the bladder base, trigone, and bladder neck, and ensure adequate sampling of the muscularis propria. Oncologic criteria for POSRC include unifocal organ-confined ≤cT2 tumor that is away from the bladder neck or trigone. The primary oncologic contraindication for POSRC and ONB is the presence of urothelial carcinoma at the urethral margin on intraoperative frozen section at the time of radical cystectomy. Relative contraindications include palpable tumor on bimanual examination and preoperative hydronephrosis.
for GST 85 PBE Jig Saws Spares - 2 600 100 575. Spare Drawing no : 25. Brand: Bosch. by Ultimamac Services Pvt. Ltd. M.R.P.: ₹ 140. Price : ₹ 118.64 Exclusive ...



 Neil
Neil 
 Neil
Neil