Ginkgo Biloba 6000 30 v tablet - 6000/30
We found that heart and lung transplant patients constitute an older subgroup of general surgical patients. These patients also undergo more than 1 procedure while admitted and often have a prolonged length of stay, consistent with transplant patients having more comorbidities [13]. Our study shows that some procedures such an inguinal/femoral hernia repair can by performed safely in either population. For small bowel resections, the outcomes are similar in transplant and nontransplant populations unless there is a delay to surgery. Prior studies have demonstrated that conditions warranting small bowel resection are complex and carry excess morbidity whether or not immunosuppression and transplantation are involved [14]. Results from our study show that for other procedures such as appendectomies, cholecystectomies and abdominal exploration, there is considerable morbidity in heart and lung transplant patients.
The Nationwide Inpatient Sample (NIS) database is currently the largest database of all-payer inpatient data [5]. The database is a stratified sample of approximately 20% of US hospitals and contains information on more than 8 million hospital stays per year. This large sample size represents roughly 95% of all hospital discharges and enables analysis of specific patient populations [5].
Statistical analysis of categorical variables was performed using χ2 tests, and cohort comparison was performed using t tests and analysis of variance. All data analyses were performed using STATA v.14 (College Station, TX) [9].
We would like to acknowledge all of the HCUP Data Partners that contribute to HCUP (www.hcup-us.ahrq.gov/hcupdatapartners.jsp). We appreciate Patrick Hilden, MS, who provided statistical input to our manuscript.
Despite these limitations, our study is the first ever to report a population-based analysis of general surgical outcomes in heart and lung transplant patients with a meaningful sample size. We conclude that all general surgical procedures should not be taken lightly in this population given the increased potential for morbidities and prolonged length of stay.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
NIS obtains inpatient data from hospital discharge abstracts and billing records and is able to provide patient demographics, hospital length of stay (LOS), morbidity, in-hospital mortality, and inpatient diagnosis and procedure codes using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). The database also provides sampling weights that allow calculation of national estimates. Approval for the use of the NIS data in this study was obtained from the Healthcare Cost and Utilization Project (HCUP) [5].
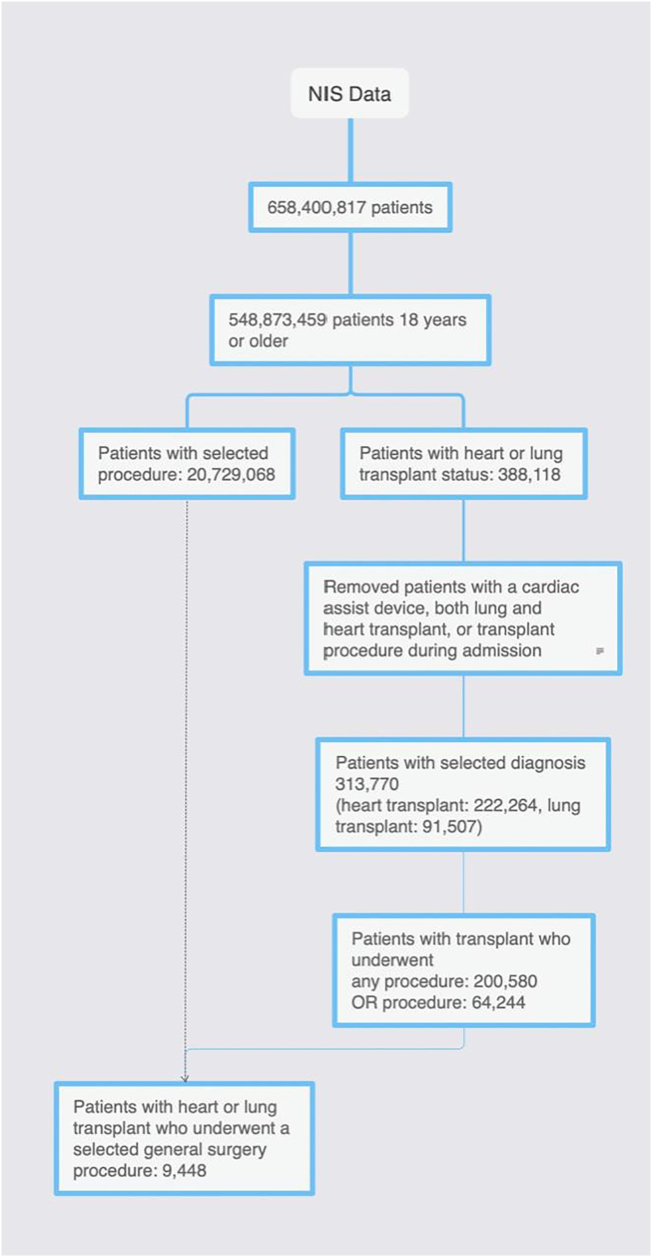
Using the NIS database from 1998 through 2015 Q3 (NIS transitioned from ICD-9 to ICD-10 in Q3), all inpatient hospital encounters for patients undergoing a general surgery procedure, regardless of transplant status, were extracted [5]. These encounters were then stratified by transplant status into “transplant” (heart or lung transplant) and “nontransplant” cohorts. Admissions under the age of 18 years, with incomplete data, those who had a cardiac assist device, both a heart and lung transplant, or who underwent a transplant procedure during the admission were excluded from analysis. Additionally, if during analysis a sampling stratum contained only 1 sampling unit, it was excluded. A CONSORT diagram demonstrates how the study population was derived (Fig 1).
Diagnosis and procedural codes were selected using the ICD-9-CM. Transplant status was identified using diagnosis codes V42.1 (heart transplant) and V42.6 (lung transplant). Procedures considered “general surgery procedures” included appendectomies, cholecystectomies, inguinal hernia repairs, small bowel resections, and large bowel resections. For a comparator group, patient admissions for the same procedures in a nontransplant group (excludes all solid organ transplant including heart, lung, kidney, liver, small bowel) were also identified. Both open and laparoscopic procedures were included except for inguinal hernia repairs, which included only open procedures. Appendix A lists all ICD-9-CM codes used.
Our findings demonstrate that heart and lung transplant patients, compared to nontransplant patients, have more complications and a higher length of stay after certain general surgery procedures.
Heart and lung transplant recipients will often need extra surgical procedures. The morbidity and mortality of common general surgery procedures such as appendectomy, cholecystectomy, hernia repair, and colon and small bowel resection in this patient population are not well known. Lung and heart transplant patients may travel to select centers for transplantation but might require general surgery in their more immediate hospitals. As studies have been limited to case series from select centers [3,4], we sought to better characterize the outcomes of heart and lung transplant patients who undergo general surgery by examining a national database.
Corresponding author at: Department of Surgery, RWJBarnabas Health, Saint Barnabas Medical Center, 94 Old Short Hills Rd, Livingston, NJ 07039. Tel.: + 1 973 322 2224; fax: + 1 973 322 8565. Amber.Turner@rwjbh.org
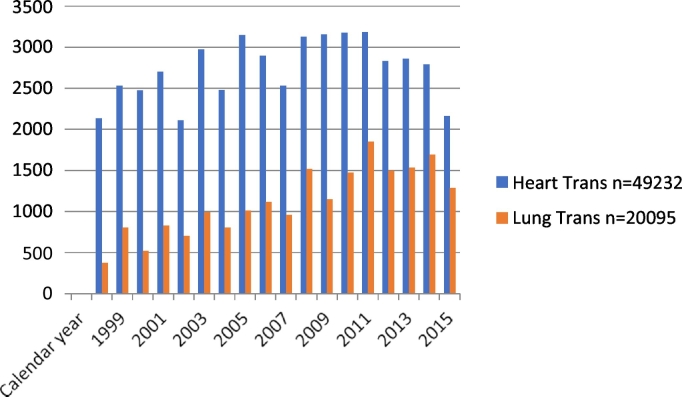
General surgery procedures remained relatively constant for heart transplant patients from 1998 to 2015 but steadily increased for lung transplant patients (Fig 2). The majority of both heart and lung transplant patients underwent general surgery procedures as nonelective cases (57% and 58%, respectively). The most common general surgery procedures in heart and lung transplant patients were cholecystectomy (38%, 38%), colorectal resection (19%, 25%), and lysis of peritoneal adhesions (11%, 14%) (Table 2). While admitted in the hospital, heart and lung transplant patients undergoing general surgery procedures had more than 1 procedure compared to the nontransplant group.
Although most patients were discharged home after surgery, transplant patients had lower rates than nontransplant patients (Table 2). Mortality rates were higher in the heart and lung transplant patients compared to the nontransplant group (4% vs 2%, P < .001 and 5% vs 2%, P < .001 mortality, respectively). Overall complication rates for all general surgeries had greater variability. Heart transplants had the lower rate of total complications, whereas lung transplants had the highest (9% heart transplant, 13% lung transplant, 11% nontransplant). Disparities also existed between the groups for length of stay. Transplant patients were more likely to have longer median LOS in the hospital (6 days for both heart and lung transplant patients) versus nontransplant patients (4 days, P < .0001, Table 2). There were also more heart and lung transplant patients who had prolonged length of stay of 30 days or more than nontransplant patients.
We certify that all individuals who qualify as authors have been listed; each author has participated in 1 or more of the following areas: conception and design of this work, the acquisition and/or analysis of data, and the writing and/or critical revision of the document. All contributing authors approve of the submission of this version of the manuscript and assert that the document represents valid work. If information derived from another source was used in this manuscript, we made appropriate acknowledgments in the document. All contributing authors take public responsibility for this work.
Patient demographics extracted included age, sex, ethnicity, household income quartile, insurance status, and discharge disposition. Baseline comorbidities were identified using the Elixhauser classification system [6]. Primary outcome measures included the postsurgical mortality, postsurgical morbidity, and hospital length of stay for nontransplant, heart transplant, and lung transplant patients undergoing the same procedures. We performed pairwise comparisons between the nontransplant cohort and either the heart or lung transplant cohort. Postsurgical mortality was defined as a patient who died after surgery but before being discharged from the hospital because the NIS database does not include any readmission or postdischarge information. Postsurgical morbidity was defined using select using codes from the ICD-9-CM and categorized as either a cardiac, pulmonary, operative, or infectious complication. Secondary outcomes were length of time in days between admission and surgery and whether a delay, defined as time greater than median time from admission to surgery, was associated with increased morbidity or mortality.
We determined the median time from admission to surgery for 4 select procedures for nontransplant patients, heart, and lung transplant patients (median time nontransplant, heart transplant, lung transplant), respectively: cholecystectomy (1, 1, 1 day), appendectomy (0, 0, 0 day), small bowel resection (1, 1, 1 day), and colorectal resection (0, 1, 0 day). Delay in surgery was defined as a surgery that occurred after the median time to surgery for that specific procedure. As shown in Table 4, mortality was only increased in patients undergoing small bowel resection whose surgery was delayed greater than the median time determined. Multivariable logistic regression using comorbidities, age, hospital size, and transplant status revealed that hospital size and comorbidities were predictors of mortality for patients undergoing cholecystectomy, appendectomy, small bowel resection, and colorectal resection. Transplant status was not found to be a predictor (Table 5).
Overall mortality was higher and length of stay longer in the transplant group compared to the nontransplant group. Analysis revealed that hospital size and comorbidities were predictors of mortality for patients undergoing certain general surgery procedures. Transplant status alone did not predict mortality.
Improved immunosuppressive medications and continued experience in transplantation have resulted in heart and lung transplant recipients living longer. With improved survival, heart and lung transplant patients are at higher risk of being inflicted with conditions that require general surgery [10,11]. Although the index general surgery operation may not necessarily differ between immunocompetent and immunocompromised patients, the ability of transplant patients to recover from complications is limited. Smith et al showed that, in lung transplant patients requiring abdominal surgery, time to surgery of longer than 6 days appeared to be associated with mortality [12]. Our goal was to find guidance on whether these patients should be transferred to tertiary care facilities for their general surgical care or if their acute issues could be dealt locally, avoiding unnecessary travel and delay in treatment. Our study is the first to use a population-based analysis to determine outcomes after such procedures. Our findings are more generalizable than those of previous case series that only report findings from select centers.
Examining specific surgical procedures, small bowel resections had the highest complication rates overall (> 45%) for both transplant and nontransplant patients (Table 3). Transplant patients who had either a cholecystectomy or appendectomy also had higher complication rates. Pulmonary and cardiac specific complications were significantly higher in heart and lung transplant patients versus nontransplant patients in those patients undergoing cholecystectomy, appendectomy, and colorectal resection. Heart transplant patients who had an appendectomy had a 3% operative mortality compared to 1% for nontransplant patients, P = .002. Transplant and nontransplant patients had a similar complication profile after hernia repair, with heart transplant patients having fewer cardiac complications than nontransplant patients (6% vs 15%, P = .003). Compared to nontransplant and heart transplant patients, lung transplant patients had significantly higher complications (cardiac, pulmonary, and infectious) as well as prolonged length of stay after a lysis of adhesions procedure (Table 3).
Categorical variables are reported as weighted counts and percentages, whereas continuous variables are reported as ranges or means/medians. Per NIS guidelines, values that contain counts of 10 or fewer were omitted [5]. A P value of < .05 was considered statistically significant. All reported P values are 2-sided.
We recognize that there are several limitations to our retrospective data set analysis. Our study is limited to only short-term inpatient outcomes, and postdischarge outcomes such as readmission are not known. The study encompasses 17 years, in which practices may have changed. Because of the small sample size, it was not possible to examine the impact of minimally invasive surgical techniques or volume outcome relationships. Additional factors, such as the specialty training and board certification of the operating surgeon, are not known within the NIS data set, which may be an important determinant of quality of care. We also found that transplant status was not an independent predictor of outcome. We feel that transplant status is a surrogate for comorbidities which are more prevalent in transplant patients. Hence, this may be a construct of our statistical analysis and be a predictor in other models where as many comorbidities are not included. Another limitation is that we are unable to identify when the transplantation occurred, therefore rendering it more difficult when factoring in comorbidities and immunosuppression. Finally, because NIS data are deidentified, hospital admissions rather than individual patients were analyzed. It is therefore possible that a transplant patient may have had more than 1 hospital admission. Given the size of the transplant population (388,118 encounters), NIS's sampling strategies, and variability in patient demographics, this is expected to be a rare occurrence and is adjusted for by not reporting on groups with fewer than 10 individuals.
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Higher morbidity and greater number of operations required for similar diagnosis suggest the higher complexity of similar abdominal problems in thoracic transplant patients. This may not necessarily be a function of their prevalent level of immunosuppression but more likely is a function of cumulative effect of immunosuppression over the lifetime of the transplant. Managing the same disease process in a transplant patient may require one to lean toward being more conservative and choose early operative intervention as opposed to percutaneous temporization interventions. Similarly, intraoperatively, in our practice, we have noticed that surgeons take a more conservative approach in transplant patients, such as use of nonabsorbable sutures for fascial closure and greater use of alimentary tract diversion rather than primarily reestablishing continuity. Prior experience in managing this patient group could be invaluable when facing such a presentation.
Analyses were performed with raw numbers and weighted by sampling hospitals and strata to reflect national averages [7]. Binary and categorical variables were compared using the likelihood-ratio test statistic for proportions, which was corrected for survey design using the second-order Rao and Scott correction [8]. Continuous variables were compared using 2-sample t tests with unequal variance. A multivariate logistic regression with multiple comparisons correction was used to derive factors and their relative weight on postsurgical mortality. Independent variables used for risk adjustment included demographics (age, sex, and ethnicity), hospital size, and Elixhauser comorbidities.
Heart and lung transplantation has become the standard of care for many eligible patients with end-stage cardiac and pulmonary disease [1,2]. Transplantation rates are now mainly limited by the availability of suitable donor organs. Long-term outcomes have improved as centers have accumulated expertise in managing immediate postoperative complications of transplantation as well as the long-term sequela of chronic rejection with the improved immunosuppression [1].
A total of 313,770 hospital encounters with existing transplants were identified spanning from 1998 to 2015, 222,264 admissions with an existing heart transplant and 91,507 with an existing lung transplant. From the original sample, 9448 admissions were identified having undergone a general surgery procedure, 6433 heart transplant admissions, and 3015 lung transplant admissions. We also identified 23,764,164 patient admissions for the same procedures in a nontransplant group for comparison.
Heart and lung transplant admission demographics differed significantly from the majority of nontransplant admissions demographics (Table 1). Transplant patients undergoing general surgery procedures were often older (mean age of 57 years transplant vs 51 years nontransplant) and of male sex (68% transplant vs 40% nontransplant). They were also primarily white (81% vs 70% nontransplant), and a majority were Medicare recipients (58% vs 31% nontransplant).
The National Inpatient Sample (1998–2015) was used to identify 6433 heart and 3015 lung transplant patient admissions for general surgery procedures. For a comparator group, we identified 23,764,164 nontransplant patient admissions for the same procedures. Patient morbidity and mortality after general surgery were compared between transplant patients and nontransplant patients. Data were analyzed with frequency tables, χ2 analysis, and a mixed-effects multivariate regression.
The postoperative morbidities and prolonged length of stay after some of these procedures argue that these transplant patients are better served at tertiary care centers [[15], [16], [17]]. Our analysis hinted at this, as hospital bed size was a predictor of mortality. The ability to rescue from complications is an increasing well-known factor that determines mortality. Larger institutions are likely better equipped to deal with postoperative complications as well as manage immunosuppression regimes. Specialized medical and surgical units dealing with heart and lung transplant patients can facilitate postoperative care as well as ensure that posttransplant protocols are being followed. Transfer to these specialized facilities, in our opinion, should be considered in patients, particularly if patients are stable. Patients requiring emergent operative intervention, such as that for small bowel obstruction, should not, however, be denied surgery because the patients comorbidities’ and not transplant status determine outcome.
Heart and lung transplant patients can develop conditions necessitating general surgery procedures. Their postoperative morbidity and mortality remain poorly characterized and limited to case series from select centers.



 Neil
Neil 
 Neil
Neil